Published on: August 26, 2022 | Updated on: August 29, 2024
Whenever a part of your body is impacted in any way, like being hit, pinched, or punctured, your nerves send signals to your brain that tell you that you are in pain. Nerves can get pinched or damaged anywhere in the body, which can be extremely painful and lead to permanent damage. When there is no medication for such a problem, and it is beyond the point of physical therapy (if these nerves are damaged), the one remaining solution is a procedure preventing these nerves from causing further pain.
That procedure is not a rebuilding or transplant of these nerves but a complete ‘burning’ or deactivation of them to eliminate chronic pain. Lower back pain, in particular, is among the most common types of pain that people experience when they get older, ranging from mild to feeling unable to sit.
Instances like this are when it is most appropriate to have the procedure done, but are the potential side effects worth the risk? As a minimally invasive but very effective relief to chronic pain, the risks will outweigh the outcome.
Why Burn Your Nerves?
Excessive pain signals sent to your brain can be torturous and detrimental to leading a normal, healthy lifestyle. As essentially a cure for your chronic pain, the process is exponentially more effective than any ‘ice and heat’ treatment, does not have severe side effects, and will deactivate those dreaded pinched nerves.
These are made of particular tissues and nerve fibers that act as a transit system, registering the impact point to your brain as a pain signal. This works but is not wholly devoid of complications: Nerve damage, pinched nerves, muscle tensions, compressions, or just over-sensitivity in that area can cause significant discomfort that either stays or worsens over time if left untreated.
When that occurs, this is where ablation (nerve burning) comes into play: The nerves that speak to your brain no longer can because the procedure puts those nerves under a heating current strong enough to cancel transmission to your brain. In other words, ablation is the blockage of nerve signals reaching their destination, leaving you with little to no pain.
Is it Safe?
In light of surgery or other vulnerable treatments, patients with arthritic or chronic pain often turn to the procedure for reasons beyond its effectiveness. The ease of operation, quick procedure times (usually one hour or less), non-invasive, and, of course, its safety. Burning nerves or radiofrequency ablation is fast and painless enough not to have the patient be put under and does not apply any of the procedural heat to virtually any other area except for those few targeted nerves.
Because of this, and the fact that no incisions or risk of surgical complications are involved at all, the procedure is arguably one of the safest treatments for handling chronic pain. The operation is also safe to repeat if at least three weeks have passed without burning off or damaging nerves.
Burning Nerves in the Lower Back
 On the surface, the procedure may sound like it will be painful or make things more uncomfortable, but burning your nerves is so painless and non-invasive that the method does not even require traditional anesthesia (some mild sedation may be necessary, but not enough to put you under.
On the surface, the procedure may sound like it will be painful or make things more uncomfortable, but burning your nerves is so painless and non-invasive that the method does not even require traditional anesthesia (some mild sedation may be necessary, but not enough to put you under.
To prevent the shooting pain in your lower back that you may experience (or have flare-ups) upon stretching or sitting, you could avoid those nerves from sending pain signals throughout the body in just under the time it would take a medication to work.
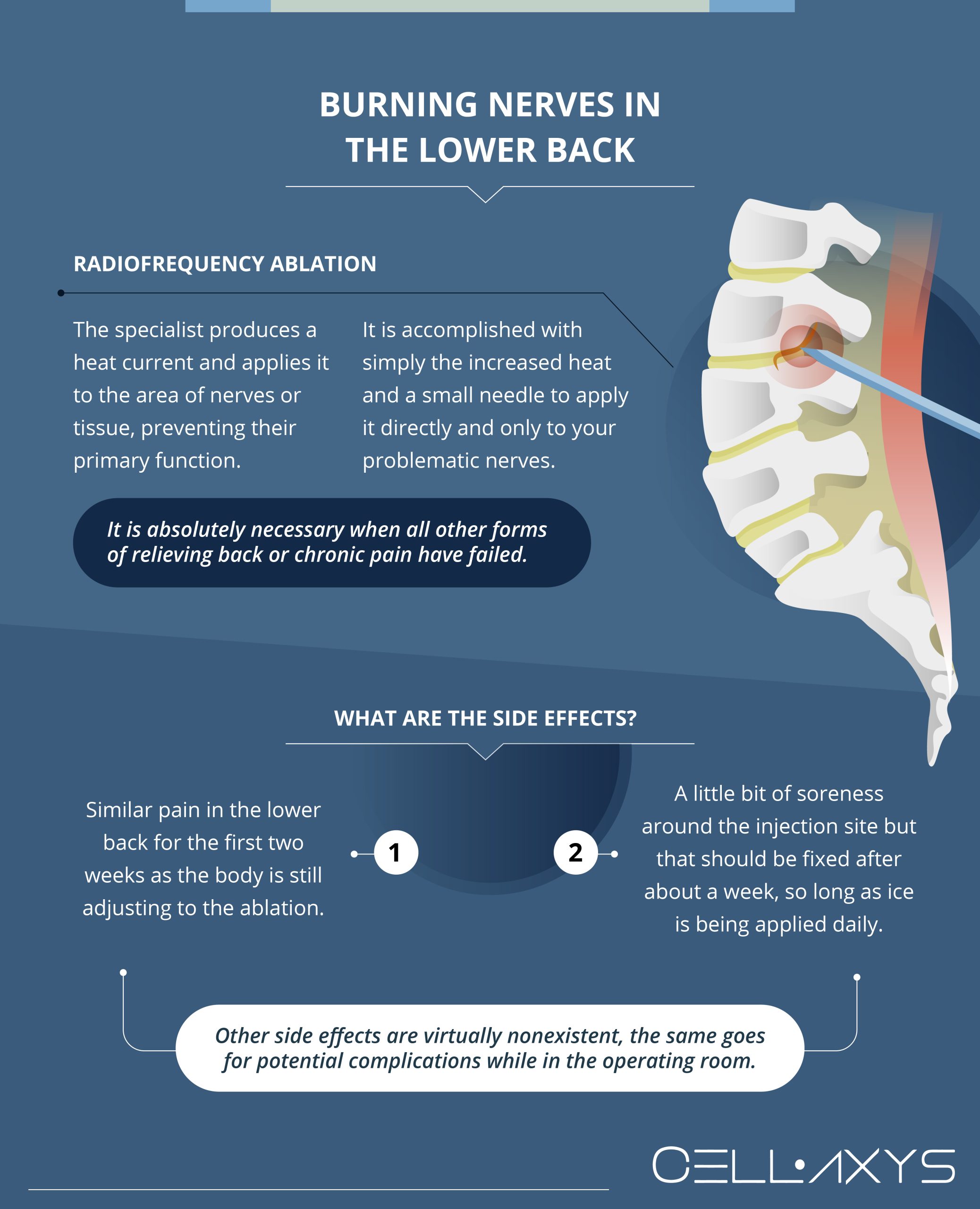
Radiofrequency Ablation
The actual burning of nerves in your lower back is radiofrequency ablation. As much as it is known to treat chronic pain, ablation (rhizotomy or fulguration) is not unusual for arthritis. When the RFA is performed, the specialist produces a heat current and applies it to the area of nerves or tissue, preventing their primary function.
Ablation is not considered surgery and can be completed with simply the increased heat and a small needle to apply it directly and only to your problematic nerves. Even nearby, not a healthy nerve gets mixed in or damaged when you are in the specialist’s care.
When is it Necessary?
Ablation is necessary when all other forms of relieving back or chronic pain have failed. While it is not a last-ditch effort to heal your pain, there are many options to fix the problem, and there is no reason to completely rule them out before trying them. It is also likely that surgery might still be necessary to correct something near the area anyway, so ablation would be a fantastic option if you cannot afford to wait during this time and your lower back pain has not been going away.
What are the Side Effects?
Thankfully, the most well-known side effects are minimal and very short-term in that the typical side effects after the procedure do not last more than one month. It is not unusual to temporarily see a similar pain in the lower back for the first few weeks as the body is still adjusting to the ablation. However, this should calm down and noticeably reduce pain after about two weeks. Beyond that, you might feel a bit of soreness around the injection site, but that should be fixed after about a week, so long as ice is being applied daily.
Other noteworthy side effects of radio ablation are virtually nonexistent. The same goes for potential complications while in the operating room.
Odds of Radiation Sickness
While an RFA does use radio frequencies internally, the procedure has not been shown to have caused radiation sickness. A few rare cases of nausea followed by chills or a mild fever are common side effects under postulations. Still, none of it is cancerous or points to any other medical condition.
How Long is the Recovery?
Ablation has one of the shortest recovery times of any non-invasive procedure. The first three days of your recovery are when doctors recommend not exerting yourself or operating heavy machinery physically, just in case you feel uneasy. Afterward, the distinctive drop in chronic pain typically occurs within two to three weeks following the procedure.
Routine checkups are always good to help keep your health in order, and checking up on the injection site after one year (if there have been no problems) is highly recommended since a few procedures are not permanent.
How the Alternatives Compare
In essence, ablation (RFA) has a fantastic success rate and arguably does more for your back and arthritic pain than these surgical alternatives, including the surgery itself. To explain, the success of ablation can range anywhere from 70%-90% depending on the situation, but even then, the procedure can be repeated if the results are not as expected.
No medication will fix nerve damage or prevent it from sending pain signals to your brain, nor will any amount of physical therapy do the same thing. The solution is a procedure that corrects the source of the pain and not just the pain itself.
Conclusion
If you are one of the millions of Americans who suffer from lower back pain and are wary of surgery or medications, you could easily find a worthwhile solution in radiofrequency ablation. Even if you are due for back or spinal surgery, an RFA is a highly safe procedure to stop the process of making pain signals to make your waiting time less painful and more bearable.
Sources
Footnotes
- Kapural L, Mekhail N. Radiofrequency ablation for chronic pain control. Current Pain and Headache Reports. 2001;5:517-25.
- Leggett LE, Soril LJ, Lorenzetti DL, Noseworthy T, Steadman R, Tiwana S, Clement F. Radiofrequency ablation for chronic low back pain: a systematic review of randomized controlled trials. Pain Research and Management. 2014;19:e146-53.
- Kim HS, Wu PH, Jang IT. Lumbar degenerative disease part 1: anatomy and pathophysiology of intervertebral discogenic pain and radiofrequency ablation of basivertebral and sinuvertebral nerve treatment for chronic discogenic back pain: a prospective case series and review of literature. International journal of molecular sciences. 2020;21(4):1483.
- McFadden SL, Mooney RB, Shepherd PH. X-ray dose and associated risks from radiofrequency catheter ablation procedures. The British journal of radiology. 2002;75(891):253-65.
References
- Radiofrequency neurotomy. Mayo Clinic. Accessed 9/6/2023.
- What to know about a pinched nerve in the lower back. Medical News Today. Accessed 9/6/2023.
- Radiofrequency Ablation (RFA) Side Effects and Risks. Spine-Health. Accessed 9/6/2023.
CELLAXYS does not offer Stem Cell Therapy as a cure for any medical condition. No statements or treatments presented by Cellaxys have been evaluated or approved by the Food and Drug Administration (FDA). This site contains no medical advice. All statements and opinions are provided for educational and informational purposes only.
Dr Pouya Mohajer
Author
Pouya Mohajer, M.D. is the Director of Spine and Interventional Medicine for CELLAXYS: Age, Regenerative, and Interventional Medicine Centers. He has over 20 years of experience in pain management, perioperative medicine, and anesthesiology. Dr. Mohajer founded and is the Medical Director of Southern Nevada Pain Specialists and PRIMMED Clinics. He has dedicated his career to surgical innovation and scientific advancement. More about the doctor on this page.
Dr Pejman Bady
Contributor
Dr. Pejman Bady began his career over 20 years ago in Family/Emergency Medicine, working in fast-paced emergency departments in Nevada and Kansas. He has served the people of Las Vegas as a physician for over two decades. Throughout this time, he has been met with much acclaim and is now the head of Emergency Medical Services in Nye County, Nevada. More about the doctor on this page.









