Published on: January 29, 2020 | Updated on: November 4, 2024
Because each surgical technique affects the body in various ways, recovery after the four main forms of back surgery — spinal fusion, artificial disc replacement, laminectomy, and discectomy – may vary.
The level of damage caused by spinal problems such as degenerative disc disease, spondylolisthesis, spinal stenosis, and other disorders of the spine has a substantial impact on recovery following these surgical operations. The amount of time a patient spends recovering after surgery is typically determined by their age and physical condition.
The surgical process used will also have an impact on your experience. Except for the time it takes to recuperate following back surgery, which can range from 3-4 weeks to a year, most patients leave home with less discomfort in their lower back or neck than they did before the procedure.
Anatomy of the Spine
The spine is one of the most important bone structures in the body. It provides support and stability during almost any activity. The spine also functions as protection for the spinal cord, a bundle of nerves that begins in the brain and ends in the lumbar portion of the spine. The spinal cord is responsible for sending many signals from the brain to the rest of the body.
There are three major regions of the spine. The cervical portion of the spine exists in the neck and upper back. The thoracic spine is located in the middle of the back. The lumbar spine exists in the lower back above the pelvis. Each region of the spine has a fixed amount of vertebrae.
Vertebrae are protected by discs that act as cushions between bones. Many spinal injuries are a result of deteriorated or dislocated discs. Some of the most common causes of back pain are:
- Bulging or herniated discs:<span style=”font-weight: 400;”> discs in the spine can come out of their normal positions and place pressure on the spinal cord. Pain is commonly felt in the area where a disc is dislocated. Treatment consists of realigning the spine and participating in fewer activities that add stress to the spine.
- Misalignment of the spine: poor posture or conditions such as scoliosis can cause microtrauma to the spine. A buildup of small injuries can lead to pain later in life.
- Arthritis: back pain from arthritis mostly occurs in the lower back. Treatments may include exercise, practicing good posture, and medication.
- Strained muscles or ligaments: some activities can place a strain on the muscles and ligaments that support the back. Strains are most often caused by activities such as lifting or bending over. Treatment for these types of injuries involves resting the muscles.
Diagnosing a Spinal Injury
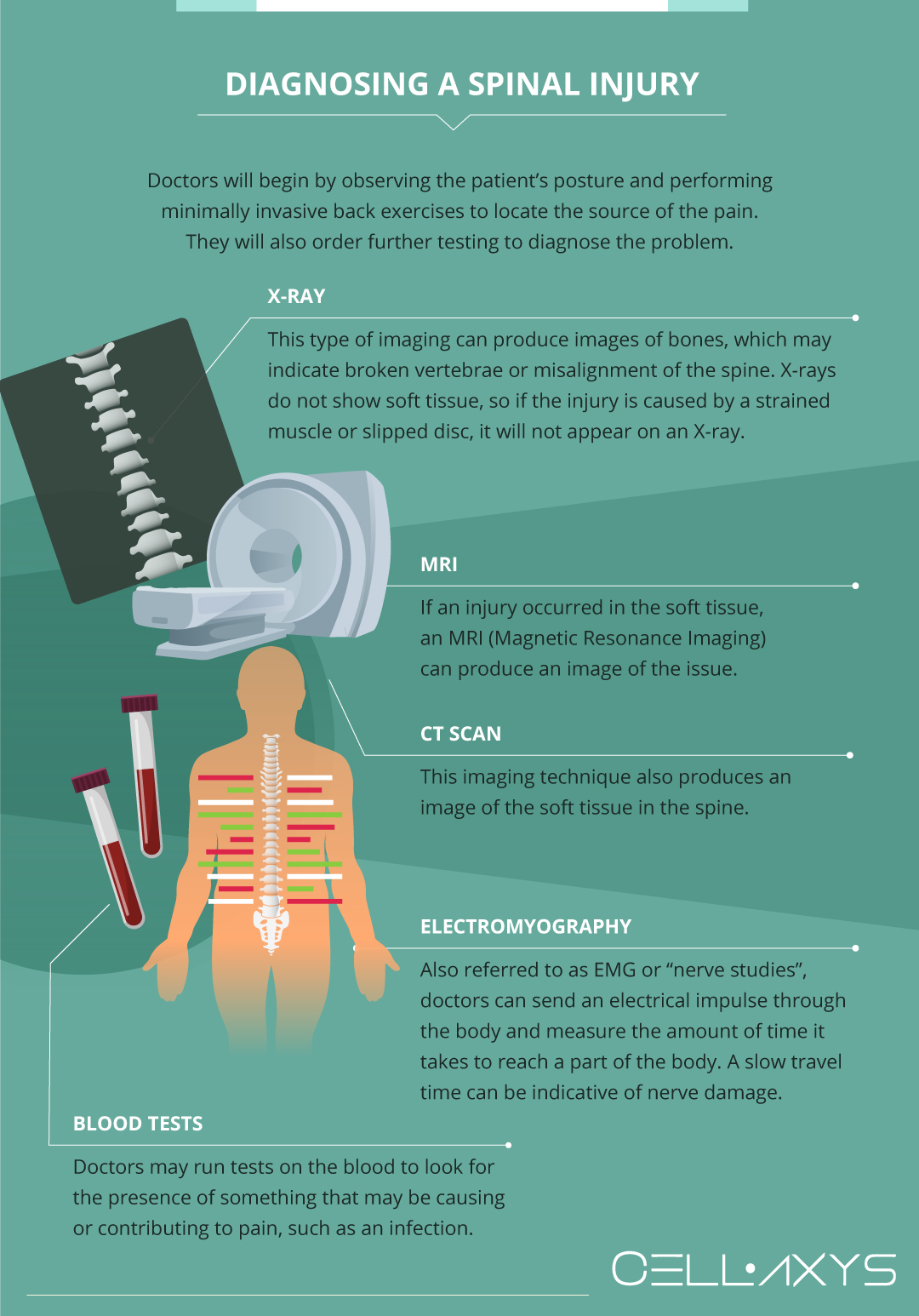
When back pain becomes too intense to perform daily activities, it is time to see a medical professional. Doctors will begin by observing the patient’s posture and performing minimally invasive back exercises to locate the source of the pain. Doctors will also order further testing to diagnose the problem. These tests may include:
- X-ray: this type of imaging can produce images of bones, which may indicate broken vertebrae or misalignment of the spine. X-rays do not show soft tissue, so if the injury is caused by a strained muscle or slipped disc, it will not appear on an X-ray.
- MRI: if an injury occurred in the soft tissue, an MRI (Magnetic Resonance Imaging) can produce an image of the issue.
- CT scan: this imaging technique also produces an image of the soft tissue in the spine.
- Electromyography: also referred to as EMG or “nerve studies”, doctors can send an electrical impulse through the body and measure the amount of time it takes to reach a part of the body. A slow travel time can be indicative of nerve damage.
- Blood tests: doctors may run tests on the blood to look for the presence of something that may be causing or contributing to pain, such as an infection.
Back pain that is diagnosed in its beginning stages can often be treated with nonsurgical methods. Healing from spinal injuries can take weeks and even months depending on the cause and an individual’s commitment to recovery.
Conventional Treatment Methods for Back Pain
Once a diagnosis has been made, doctors will create a treatment plan that is specific to each patient’s needs. Some factors that might influence treatment include overall fitness level, diabetic status, and financial flexibility, for example.
Most back injuries do not require surgery and respond well to conventional treatments such as:
- Medication: doctors may suggest over-the-counter NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) such as ibuprofen to help relieve back pain. They may also suggest prescription pain medication depending on the level of pain. These may be NSAIDs or narcotics such as oxycodone. Taking prescription pain medication should be closely monitored by a doctor as it can be dangerous.
- Muscle relaxant: medication that relaxes muscles can be a good option for an individual who has suffered from a strain or whose spine has become misaligned.
- Corticosteroid injections: one option for individuals who have back pain is corticosteroid injections. Doctors inject a powerful synthetic dose of the hormone cortisol, which can relieve pain in the short term. These injections have proven to damage soft tissue over time, however, so they should be closely monitored by a doctor.
- Heat and salves: some pain relief can be found by applying heat to the affected area. Some individuals also elect to try topical pain relief in the form of lotions or salves.
- Physical therapy: one of the most successful treatments of back pain is physical therapy. This works well for many patients because physical therapists work with the patient’s specific needs. Physical therapists can inform patients of what exercises they can do to relieve pain at home, as well as things like what sleeping position is best for their condition. Physical therapy may last weeks or months depending on the patient’s progress.
- Surgery: most individuals who experience back pain do not need to consider surgery, as conventional treatments are often enough to relieve pain or fix the underlying problem. If a patient goes 6 months without significant improvements, however, doctors may consider surgery. Some of the most common types of surgery for back pain include:
- Spinal fusion: this form of surgery involves removing the problematic disc and fusing two vertebrae. Spinal fusion is considered major surgery and can have a recovery period of 6 months to a year. Most doctors will recommend other surgeries before considering spinal fusion, as it is seen as a last resort for treating back pain.
- Artificial disc replacement: doctors may recommend a disc replacement surgery. A surgeon removes the problematic disc and replaces it with a synthetic disc made of metal and plastic. As this surgery is less invasive than spinal fusion, the recovery time is shorter – about 2-3 months.
- Laminectomy: this type of surgery involves cutting bone or muscle that is placing pressure on the spinal cord so that the nerve is no longer under stress. This is the least invasive form of spinal surgery. The recovery time is under 2 months.
- Discectomy: is the most popular procedure for addressing neck pain caused by a degenerative or herniated disc. The troublesome disc is completely removed and replaced with a bone graft (or bone graft replacement) to allow the neighboring vertebrae to fuse over time.
Making the Decision
Before surgery, it is important to maintain an open dialog with medical professionals so that any questions can be answered and recovery is as quick and painless as possible.
Many factors may influence a patient’s decision to undergo surgery, including money, taking time off of work, the extent of daily disruption, and support system. Knowing what to expect before, during, and after surgery can be extremely beneficial to a patient. Being aware of what exactly is going to happen and the potential risks can greatly ease any anxiety or stress that comes with making the decision.
Understanding the risks of surgery is important – these include infection, blood clots, or a reaction to anesthesia – though there may be more risks that are important to discuss with professionals.
Spinal Surgery Recovery Timeline
Recovering from back surgery is a long process requiring patience, discipline, and focus. No matter which kind of surgery you’ve had, whether it is spinal fusion, discectomy, or laminectomy, understanding the surgery and the recovery process is crucial to have a smooth healing process.
Let’s look at the recovery process in stages.
Preparing for Surgery
Some steps need to be taken before the surgery begins. This may include taking time off of work, arranging a ride home from the hospital, scheduling blood work, and packing an extra change of clothes.
Some surgeries require that the patient not eat or drink for a certain period before the operation. Be sure to learn precisely what is expected within the week before surgery.
Stage #1: Immediate Post-Surgery Phase
Depending on the kind of surgery you have, your stay in the hospital may last from 1 to 3 days. If it was a complex surgery, they might keep you in for three days, but less invasive surgery requires a day of hospital stay.
There, the medical team stays active, monitors for post-surgical complications, and helps you regain mobility after surgery.
They will keep tabs on any signs or symptoms that may develop which indicate surgical complications such as
- Infections like swelling, fever, or redness
- Formation of blood clots
- Nerve damage and restrictions in movement, if any
During the first few days, there will be a lot of pain. Of course, it will be managed with medicines like NSAIDs, anesthetics, and opioids.
The physical therapist will help you sit up and walk a couple of hours after surgery. This is done to keep the blood flowing through the body and minimize the risk of blood clot formation.
You will be encouraged to use a walker, cane, or other assistive equipment.
Stage #2: Early Recovery Phase
Early recovery will be encouraged at home, where you must follow specific instructions from your surgeon.
For instance, you cannot bend, twist, or do heavy lifting or other strenuous activities. Also, take good care of the incision site, keeping it dry and clean to prevent it from getting infected. You must inform your doctor immediately if you notice any redness, discharge, or swelling.
Remember, though, that slight pain and swelling are to be expected. Use ice or heat therapy as instructed. Ice helps reduce the swelling, whereas heat minimizes stiffness.
You can also wear a brace or support to stabilize the spine during early recovery. Other things you can do to speed up recovery are:
- Go for short walks
- Do some gentle exercises that don’t strain the spine
- Do deep breathing exercises that encourage the flow of oxygen to the healing tissues
Stage # 3: Mid-Recovery Phase
The months 2-3 after the surgery or the weeks 4 to 12 will be more about improving mobility and activity.
You can then return to your daily routine and undertake light activities like short errands, house chores, etc.
At this stage, physical therapy will become more advanced, and more activities and exercises will be planned to strengthen the core and muscles around the spine.
This way, you will feel your back getting stronger so that you can do some heavy lifting later on. But at this stage, avoid lifting weights as it will risk damaging the tissues healing around the spine.
However, if you experience pain, stiffness, swelling, slow recovery, or increasing pain, you must consult your surgeon and physical therapist to redo your recovery plan.
Stage # 4: Full Recovery
After three months, you can return to your regular activities and move about like you used to. However, listening to your body and taking it easy on strenuous activities is still important.
You may go for walking, cycling, and swimming, which are low-impact exercises, but your surgeon will guide you about specific activities that can be dangerous, so make sure to avoid those.
You may even be able to go back to work if you have a desk job for 4 to 6 weeks. However, you should continue physical therapy to regain your strength and flexibility. It’ll also help improve your posture.
The Procedure
An anesthesiologist will be present to apply general anesthesia, and possibly local anesthesia to help with pain in the hours after surgery. The biggest risks of anesthesia are stroke, blood clots, and pneumonia. An IV will be placed in the arm, and a catheter will be used. Some patients have a tube inserted into the spine to drain excess fluid.
2-4 Hours After Surgery
Patients who have undergone surgery are placed in a “recovery room” until the anesthesia wears off and they wake up. Once awake, they are taken to their hospital rooms. Depending on the patient’s condition, certain exercises may be recommended to help maintain strength.
During this time, many medical professionals, such as nurses and physiotherapists working on a long-term recovery plan, may visit. Some patients may receive instructions for breathing exercises that will be helpful throughout the process.
6 Months After Surgery
At this point, most physical activity can be resumed, even if it is strenuous. However, be sure to consult with a physiotherapist or doctor before attempting the strenuous activity.
12-18 Months After Surgery
The area operated on should be fully healed after 18 months.
Some factors that may impact the recovery timeline include age, obesity, diabetes, and smoking status. These factors can slow the recovery process, but staying dedicated and consistent with physical therapy can improve the odds of a full recovery.
Recovery can be difficult, both physically and mentally. Regenerative medicine may offer hope for a less painful and faster recovery. In some cases, it can even prevent the need for surgery altogether.
The Role of Regenerative Medicine in Spinal Surgery
The burgeoning field of regenerative medicine seeks to enhance a patient’s naturally occurring cells. Using cell-based or platelet-rich plasma (PRP) therapies, some doctors can treat issues such as back pain before surgery is necessary. These treatments can also be used for pain relief after surgery.
The two types of regenerative therapy offered at CELLAXYS are:
Cell-based Therapies
Cell-based or stem cell therapies extract the patient’s cells or “autologous” tissues and reinject them into the injury site.
When the doctor harvests healthy cells from the adipose (fat) tissue, the process is called a Minimally Manipulated Adipose Tissue (MMAT) transplant. They can also remove highly concentrated cells from your bone marrow, called Bone Marrow Concentrate (BMAC). These healthy tissues stimulate the recovery process.
Platelet-Rich Plasma Therapies
In platelet-rich plasma (PRP) therapy, the blood is drawn from the patient, placed in a centrifuge to separate platelets, and reinjected into the surgery or injury site.
Platelets are the healing components that contain 10 Growth Factors to stimulate the development of healthy tissues. They also release chemical signals to attract healthy cells from the blood and produce a web-like structure called fibrin. An injury could heal faster with a high number of platelets.
Cell-based therapies are completed within 1.5 to 2 hours, while PRP takes 45 minutes. Both are outpatient procedures, meaning you can go home after the treatment. The doctor uses live X-rays and ultrasounds to spot the transplant location.
Some patients experience pain at the injection site, but this typically goes away in a matter of days. These therapies are used not only to relieve pain but also to help the body heal more quickly. There is a relatively low risk as they use the patient’s own tissue. Relieving pain with regenerative medicine can also make it easier to complete physiotherapy.
Sources
Footnotes
- Lewandrowski KU, Ransom NA, Yeung A. Return to work and recovery time analysis after outpatient endoscopic lumbar transforaminal decompression surgery. Journal of Spine Surgery. 2020;6(Suppl 1):S100.
- Wainwright TW, Immins T, Middleton RG. Enhanced recovery after surgery (ERAS) and its applicability for major spine surgery. Best practice & research Clinical anaesthesiology. 2016;30(1):91-102.
- Perrot S, Allaert FA, Concas V, Laroche F. “When will I recover?” A national survey on patients’ and physicians’ expectations concerning the recovery time for acute back pain. European Spine Journal. 2009;18:419-29.
- Skolasky RL, Mackenzie EJ, Wegener ST, Riley III LH. Patient activation and functional recovery in persons undergoing spine surgery. JBJS. 2011;93(18):1665-71.
- Pountos I, Panteli M, Walters G, Bush D, Giannoudis PV. Safety of epidural corticosteroid injections. Drugs in R&D. 2016;16:19-34.
References
- A guide to the spinal cord: Anatomy and injuries. Medical News Today. Accessed 2/23/2024.
- Lumbar decompression surgery. NHS. Accessed 2/23/2024.
- How Long Does It Take to Recover from Back Surgery? Healthline. Accessed 2/23/2024.
- Tips to Help You Recover From Back Surgery. WebMD. Accessed 2/23/2024.
CELLAXYS does not offer Stem Cell Therapy as a cure for any medical condition. No statements or treatments presented by Cellaxys have been evaluated or approved by the Food and Drug Administration (FDA). This site contains no medical advice. All statements and opinions are provided for educational and informational purposes only.
Dr Pouya Mohajer
Author
Pouya Mohajer, M.D. is the Director of Spine and Interventional Medicine for CELLAXYS: Age, Regenerative, and Interventional Medicine Centers. He has over 20 years of experience in pain management, perioperative medicine, and anesthesiology. Dr. Mohajer founded and is the Medical Director of Southern Nevada Pain Specialists and PRIMMED Clinics. He has dedicated his career to surgical innovation and scientific advancement. More about the doctor on this page.
Dr Pejman Bady
Contributor
Dr. Pejman Bady began his career over 20 years ago in Family/Emergency Medicine, working in fast-paced emergency departments in Nevada and Kansas. He has served the people of Las Vegas as a physician for over two decades. Throughout this time, he has been met with much acclaim and is now the head of Emergency Medical Services in Nye County, Nevada. More about the doctor on this page.









