Last updated on November 8th, 2023
Introduction
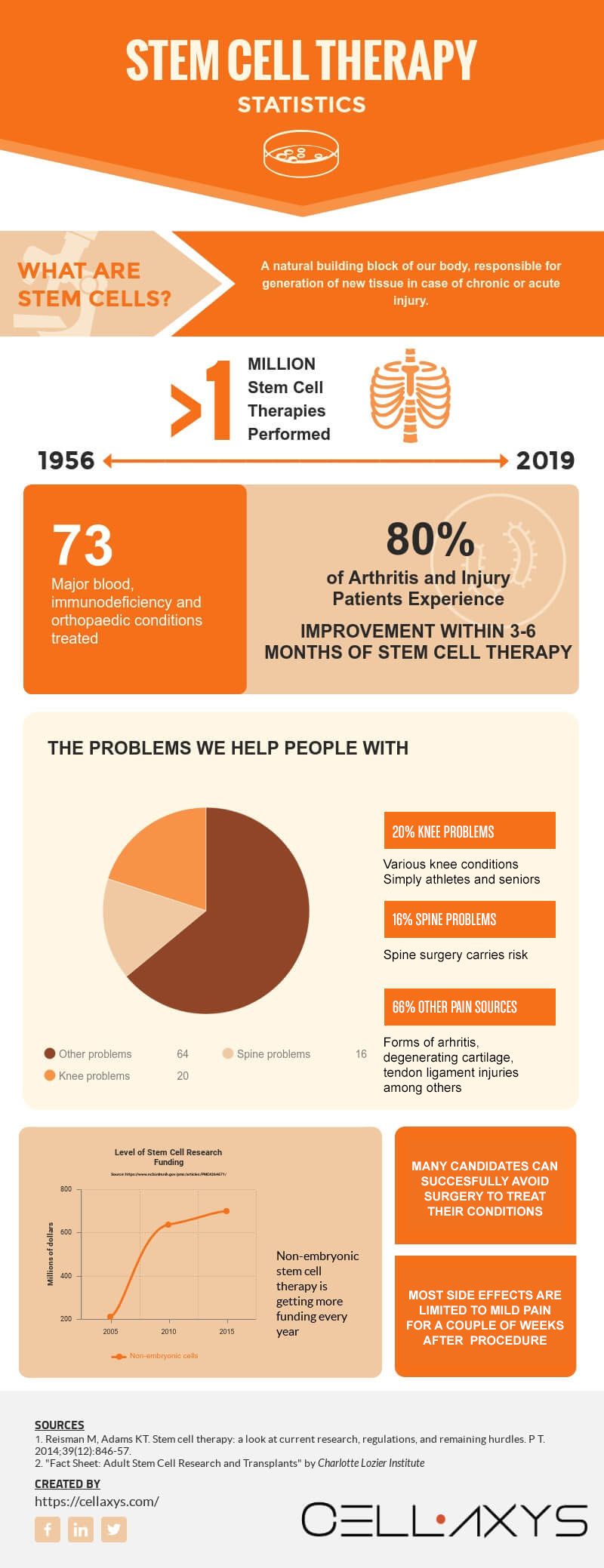
When it comes to stem cells—especially stem cell therapy—there are a few waves of shock our patients and readers usually go through.
The first big revelation comes when you realise that stem cells aren’t some magical new invention—it’s a natural building block of our bodies. In a very rough generalization, each and every one of us was once just a handful of stem cells.
The second surprise is when you learn that stem cells can be obtained from your own body, and that they can transform into several types of mature cells that your body needs to heal and regenerate.
The third wave of shock arrives when you realize that this isn’t some sci-fi movie script; tens of thousands of patients are already living proof of how transformational regenerative medicine can be. That’s right—regenerative. As in, able to regenerate damaged tissue.
Regenerative medicine | rɪˈdʒɛn(ə)rətɪv ˈmɛdɪsɪn |: the most recent and emerging branch of medical science, deals with functional restoration of specific tissue and/or organ of the patients suffering with severe injuries or chronic disease conditions, in the state where bodies own regenerative responses do not suffice.
Why haven’t you heard about this before?
In the grand scheme of things, stem cell therapy is still relatively new. More importantly, it’s still rapidly evolving.
While it’s been used by practitioners for roughly 50 years now, it was mostly blood cancer cases that seemed to have a positive response to stem cell treatment.
It wasn’t until recently that practitioners have proved how universally effective stem cells can be in regenerating tissue after injuries or restoring the effects of natural wear-and-tear.
Part I: What Is Stem Cell Therapy, Exactly?
Our bodies are made of cells.
Muscle cells construct the muscle tissue. Nerve cells are the building blocks for the nervous system. In other words, all of the cells in our body have a specific set of functions.
Except stem cells. Their job is to regenerate other types of cells, should the need occur.
What Are Stem Cells?
Stem cells are the silent hero that continuously repairs and regenerates all of our body parts. They act as the “source” that generates new, specialized cells, which can quickly adapt to an injury or natural wear-and-tear.
It can be a bit of a confusing subject, so why don’t we kick things off with an analogy?
For example, think of a stem cell as a young human being.
As a child, you have complete freedom over what you can become. You can choose to be a physics teacher, play in a professional soccer team, or to head a successful business.

Over time, you make choices based on your decision. Young professors will read a lot of books, aspiring athletes will enroll to their local soccer team, and the entrepreneurs will open lemonade stands.
Enough time passes, and each of these kids will no longer have the same freedom of choice—they will be specialized.
The teacher could never learn to kick the ball as well as the soccer player, who could never build a multi-million dollar business. Each of them would be effective in their own areas, but they would have lost their ability to change function.
Stem cells behave very similarly.
One of the main properties of a stem cell is that they can transform into any other type of cell, taking on its functions and properties.
Namely, there are 7 main types of body cells:
- Bone cells. These form combinations of collagen and calcium phosphate minerals, which, in turn, form our bones and the skeletal system.
- Blood cells. Red blood cells, white blood cells and platelets ensure the proper functioning of our body—from transporting oxygen to fighting infection.
- Muscle cells. These form muscle tissue, which enables body movement and supports our skeletal system.
- Fat cells. Also known as adipocytes, these cells store energy, produce hormones and regulate blood pressure.
- Skin cells. Coming together to form dermis and epidermis (skin tissues), these cells regulate hydration, control body temperature and prevent body organs from external damage.
- Nerve cells. A basic building block of our nervous system, nerve cells transmit signals throughout our body and into the brain.
- And… stem cells. These act as the regenerative building blocks, repairing damaged tissue all over the body.
A stem cell can become any one of these cells. Once they do, they reach maturity and function as the designated cell type.
In fact, this regenerative process happens all the time without us knowing.
Stem Cell Fact #1: Stem cells are already in our body
One of the common myths we hear is that stem cells are some new invention that scientists have mixed in their laboratories, and are now looking to inject into poor test subjects as a part of their grand experiment with the human race.
While some stem cells used in therapy do come from ‘external sources’ (read: not from your own body), we’d like to emphasize that stem cells are a natural building block of our bodies. They’ve always been there—we just weren’t aware of what they do and how to use them in therapy.
Current practical and academic research shows that stem cells are present in the:
- Brain. A small handful of stem cells are found in our brains. Their function is to repair is to generate new neurons[1] (e.g. after brain injury) and provide a supportive layer between the brain and the fluid covering the brain.
- Bone Marrow. MSCs reside in Bone Marrow. MSC are the Orthopedic and Spine stem cell. Inside our bones resides a spongy tissue, responsible for the generation of new blood cells[2].
- Adipose tissue (fat). Another rich source for therapy-effective stem cells, adipose tissue-derived stem cells (ADSC’s) play a key role[52] in reconstructive and regenerative medicine.
- Blood. With bone marrow being the main “production house” for new blood cells, some stem cells are also found in peripheral blood[3], ready to take on the responsibilities of their specialized, mature counterparts.
- Muscles. Present in the skeletal muscle tissue, muscle stem cells are the emergency squad of our muscular system, ready to jump into the action[4] if any damage to the muscle tissue occurs.
- Skin. Found in the lower level of the epidermis, skin stem cells take on a number of responsibilities[5] — from regenerating hair follicles to restoring damaged skin tissue.
- Liver. Similar to their neighbors in other body parts, liver stem cells mostly deal with chronic damage to the liver tissue[6] on a daily basis.
Stem Cell Fact #2: We regenerate all the time, actually
Given that stem cells are spread all over our body, you might sense that they’re there for a reason.
The reason is that our bodies regenerate all the time without us knowing. Us and lizards, it turns out, we’re not so different after all.
Skin, for example, we regenerate fully within 2-3 weeks. As in, every month we get a new set of skin. We shed our skin seamlessly throughout the day.
Some of our inner organs also have amazing regenerative capabilities.
Liver, for example, is known to be extremely good at regenerating. So good, in fact, that it could regenerate fully from just a quarter (25%)[7] of the full organ mass.
The inner lining of our intestines, called the epithelium, regenerates fully every 5-7 days, too.
The point is—most of our body parts have innate regenerative abilities, powered by stem cells.
However, we’re not on par with the reptiles yet in the regeneration game.
Most of our body parts… they need help to regenerate properly.
That’s where stem cell therapy comes in.
Stem Cell Fact #3: Stem cells can be harvested, concentrated, and transplanted
We won’t go all technical about the mechanics of stem cells, but a couple of core things you should know before you read anything else:
- Stem cells can be transplanted. Due to their natural ability to transform into other types of cells, stem cells can be transplanted into your problem area. The cells will adapt and take on a different “identity” as if they were there since the beginning.
- Stem cells can be concentrated and activated. While many types of stem cells are a good starting point for practical use, it is the concentration and activation of the cells that has truly made it an effective therapy. Certified physicians are able to concentrate these cells to address exactly the problem you are facing.
In fact, it is three distinctive properties[8] that set stem cells apart from the rest:
- Stem cells have the ability to “self-multiply.” Remember us saying that all of us have been just a handful of stem cells at some point? Well, that wasn’t a metaphor. One of the defining qualities of stem cells is their ability to multiply in different ways. For example, bone marrow aspirate stem cells can differentiate up to 5 times, while adipose tissue stem cells can multiply up to 8 times.
- Stem cells are able to differentiate. That’s their whole point, stem cells have the ability to differentiate into specialized cells with designated functions.
- Stem cells can renew body tissues. How is this different from point #2? Well, this says that stem cells don’t differentiate without purpose—they do so to repair damaged tissue or renew our body parts.
Where do stem cells come from?
If you’ve heard stories about stem cells, they were probably about how they are harvested.
Namely, you might have heard a notion that “in order to get stem cells, you have to kill an embryo.”
Let us shed some light on the topic.
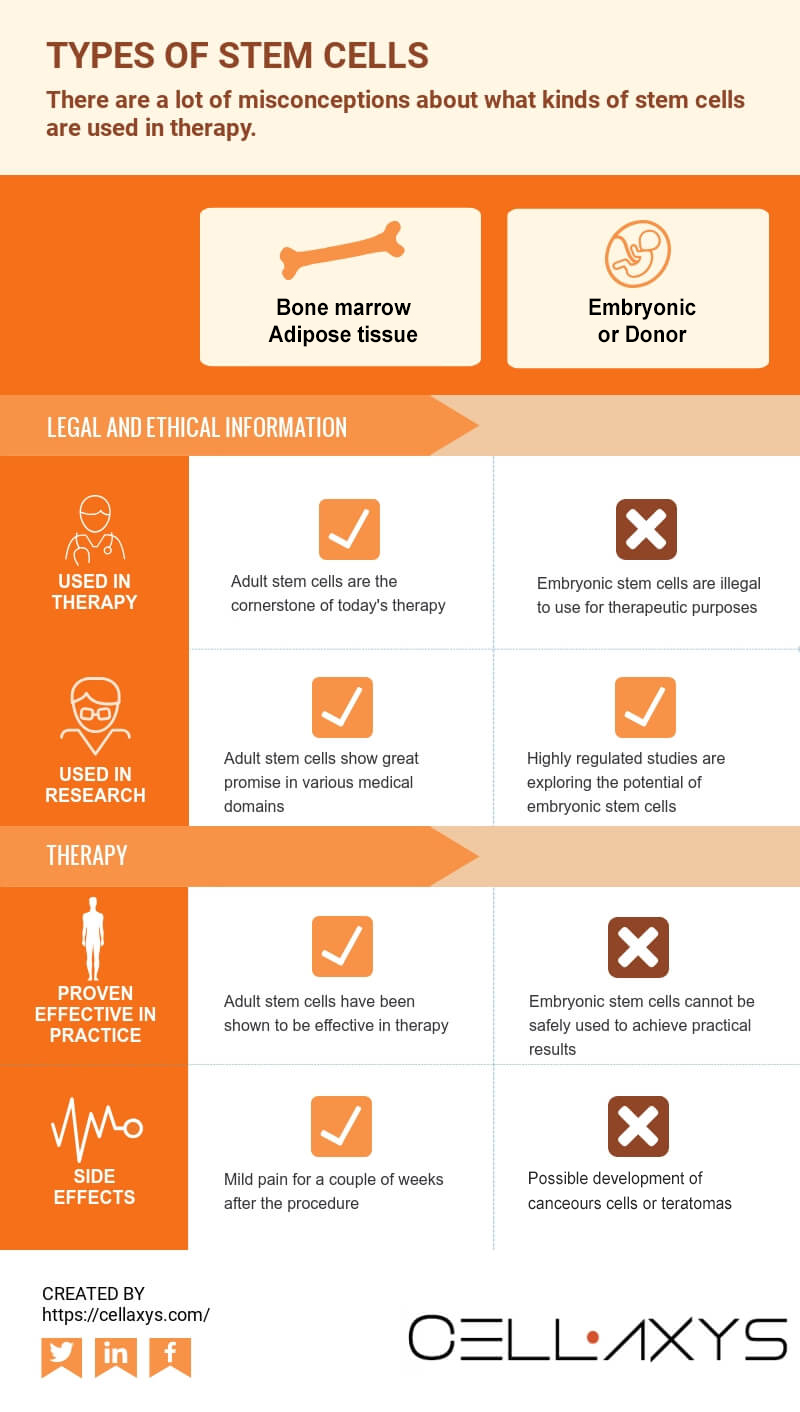
Embryonic Stem Cells
What you need to know:
- Embryonic stem cells are not used in therapy
- They’re mostly used in research
- They’re highly regulated
- Once again: they’re not used in therapy
Embryonic—or omnipotent—stem cells are at the very core of the controversy surrounding the entire area of stem cell therapy.
As their name suggests, they are gathered from embryos in the early stages of growth. They develop in eggs fertilized in in vitro fertilization[9] clinics, and are subsequently donated for research after receiving consent from the donor herself.
Scientists take particular interest in embryonic stem cells because of their vast potential. In theory, they have the ability to transform into almost any type of body cell, in unlimited quantities.
In practice, however, these cells are not used.
For one, it’s illegal to do so[10] in the US and many other countries. Only closely monitored and highly regulated research projects can use specified amounts of embryonic stem cells for experimentation.
But then, you should also know that we have not yet figured out how to use embryonic stem cells in therapy safely. Once that day comes, however, societies across the world will have important ethical questions to solve.
Adult Stem Cells
What you need to know:
- Adult stem cells are used in therapy
- They come from your own body
- Adult stem cells are the cornerstone of today’s stem cell therapy
- Sources of adult stem cells include bone marrow and fat tissue
Adult stem cells—also known as pluripotent stem cells—have been used in therapy since 1956.
Pluripotent stem cells are more limited in their differentiative and multiplicative abilities. That is, they cannot multiply an infinite amount of times, or transform into any other type of cells. There are limitations.
Major advancements in stem cell therapy are closely linked to these limitations. As we learn more about different sources of adult stem cells and about how to use them in therapy, we find new practical applications to treat diseases and injuries.
At first, scientists and practitioners have operated under the notion that adult stem cells could mostly be found in the bone marrow—a soft, spongy tissue inside our bones, responsible for generation of new blood cells.
For this reason, the first stem cell transplants addressed various blood diseases—such as leukemia. They did so successfully. (Yes, “bone marrow transplant” is also a “stem cell transplant” procedure.)
It wasn’t until 2010 that adult stem cell therapy was acknowledged as a possible solution to many of our musculoskeletal problems and a viable alternative to surgical orthopaedic treatments. Once the first person received a stem cell transplant[11] to treat spinal injury, the orthopaedic world has changed for good.
So, What Is Stem Cell Therapy?
The science behind stem cells is as complicated as is it exciting.
The therapy itself, however, is remarkably simple. That is one of its major appeals.
There are many cultural references to what stem cell therapy might one day become. The cure-all; an injection of cells that could treat any disease and heal any injury, for anyone.
Here’s how it goes in real life.
Stem Cell Therapy Procedure

Step 1: We Harvest Stem Cells
Depending on the chosen source of stem cells—whether it’s the patient’s bone marrow, adipose tissue (fat)—the first stage of stem cell therapy is to actually collect them.
With bone marrow stem cells:
- A needle will be placed into the bone marrow, and a sample will be harvested.
- Stem cells are collected from the patient’s bone marrow using a needle, typically from the patient’s Iliac crest. At Cellaxys, this is always performed under live X-ray, called fluoroscopy.
With adipose tissue stem cells:
- A small “liposuction” procedure will be performed, during which a sample of fat tissue will be harvested.
- The amount of stem cells harvested with adipose tissue varies on your individual case.
Step 2: We Concentrate and Activate Stem Cells
There is a big myth (mouthfed by marketers) that stem cells are somehow modified before transplantation.
Not only is this incorrect, it is also illegal. FDA has a clear policy[53] that only minimal manipulation[12]can be allowed in stem cell transplantation.

What exactly is minimal manipulation? Here is the answer:
- The processing of the tissue does not alter its original characteristics
- The processing does not alter any biological characteristics of cells and tissue
This is very important, because chemically or otherwise manipulating stem cells before transplantation means it’s virtually impossible to predict how these cells would predict once in the patient’s body.
It’s also important to emphasize that we do not multiply stem cells in the lab through manipulation.
All stem cells are naturally pre-programmed to divide a specific number of times:
- Bone marrow aspirate stem cells multiply up to 5 times
- Adipose tissue stem cells multiply up to 8 times
The multiplication itself can happen in lab conditions or in the patient’s body—but we have nothing to do with that. The cells themselves do the work.
So, then, what do we do before transplantation? Here is a quick rundown:
- Stem cells are concentrated using a double spin method in a highly specialized centrifuge and a required amount is prepared
- We activate stem cells with a small dose of Platelet Rich Plasma, which allows stem cells to thrive in the new environment
And that’s basically it! We don’t do any chemical or biological manipulation. Since stem cells already “know what to do”, there’s no reason to interfere with their biological structure without compromising safety.
Step 3: We Transplant Cells Into Treatment Area
This is where the true magic happens.
A concentrated sample of activated stem cells is transplanted right into where they’re needed most: the injury site or chronic illness area. This is what has proven transformative in chronic and acute musculoskeletal diseases, such as arthritis and spinal injury.
Once again, the procedure is straight forward:
- Ultrasound and X-ray techniques are used
- A concentrate of stem cells is injected right into the target area
- The patient’s recovery can vary from days to a couple of weeks
Stem cell therapy is a minimally invasive procedure. As with any procedure, there are risks involved. The physicians at Cellaxys will go over the risks, benefits, and alternative options with you during your consultation.
Want to activate your body’s natural ability to heal itself?
Consider Stem Cell Therapy.
Fill out the form below to request your FREE consultation
Why Is Stem Cell Therapy So Important? What Are The Benefits?
Stem cell therapy isn’t just a radical improvement in medicine; it’s a much needed one, too.
See, for the longest time, patient’s acute and chronic musculoskeletal injuries were faced with two groups of treatment options:
- Invasive surgical treatments, which can be risky, require a lengthy recovery period, and, sometimes, is simply not as effective.
- Alternative orthopaedic treatments—such as physical therapy or acupuncture may not provided the desired results.
The downsides of surgery are the main reason why stem cell therapy has gained so much attention recently.

Surgery Can Be Risky
Due to the invasive nature of the surgical intervention, these types of treatments can put patients at risk.
From catching an infection at the incision site to the formation of blood clots which could lead to a heart attack, surgical intervention poses an entire array of health hazards[13].
Even after hip surgery patient may continue to have pain.
One 2012 study found that as many as 35% of patients report “unfavorable long-term pain”[14] within a 5-year period after the surgery.
There are also some risks associated with hip surgery.
A more recent 2018 Finnish review discovered that as many as 4.6% of all hip surgery patients and 10% of all hip replacement patients[15] experience significant post-operational complications.
It also concluded that a number of conditions—including Parkinson’s, osteoarthritis, rheumatic diseases, and a number of mental illnesses—increase the chance of a complication.
What is more, there is an up to 3% chance for nerve damage[16] during hip replacement, and an estimated 18% chance of fracturing one of your musculoskeletal components. Patients should weigh the risks and benefits of the surgery before jumping into surgery.
Spinal surgery has also been associated with some surgical complications.
During a 2015 study of 95 test subjects who underwent lower spine surgery, 23% of them experienced significant complications[17] — including infections, blood clot formation, and nerve injury.
A similar analysis of 338 lumbar spine surgery patients found that 55 of those patients experienced complications[18] ranging from mild to severe.
Age, previous heart, and neurological conditions have all been identified as major risk factors in spinal surgery.
While hip and spine surgeries are definitely among the riskiest ones, all surgeries on any part of the body may pose some risks.
Surgery Is Not Always Effective
Given the risks, you’re faced with as a surgery candidate sometimes you do not get the results you’re looking for.
Turns out, the reality is often disappointing. Some surgery patients don’t feel like the procedure matched their expectations in terms of pain relief or mobility improvement. Sometimes, surgery can make things even worse.
For example, in 2018, a study of 26 patients tested how effective surgical treatment is for the condition called the Tennis elbow. It found that it was no more effective than placebo treatment[19].
A similar review has discovered that when treating simple elbow dislocation, there’s basically no evidence[20] that shows that surgical treatment helps those patients reduce pain, increase elbow mobility, or prevent chronic instability.
When it comes to foot surgery patients, the situation doesn’t get any better.
One study tried to gauge the satisfaction of foot surgery patients years after the procedure. Most of the patients said that the surgery failed to reduce pain or restore mobility[21].
A similar post-op follow-up[22] found that patients who felt the most pain before the surgery still feel the most pain after the surgery.
Knee surgery is a big topic among athletes and arthritis patients alike.
In 2017, a study of 140 test subjects found that most surgical meniscus repairs produced no better results than regular exercise[23].
The same year, it was discovered that a popular knee surgery—arthroscopic partial meniscectomy (APM) —has no superiority over non-surgical treatment[24]. Besides, it may cause a number of dangerous side effects (blood clots, complex regional pain syndrome, infection.)
How Does Stem Cell Therapy Compare?
The two major differences between stem cell therapy and surgical intervention are:
- Stem cell therapy is a less invasive procedure. For this reason alone, many major complications are typically less common—including blood clots.
- Stem cell therapy empowers your own body’s ability to heal. Since the stem cells used are, for the most part, harvested from your own body.
To sum up the major benefits of stem cell therapy vs. surgical treatment:
- Lower risk of major surgical complications (blood clots)
- A shorter recovery time. Most surgeries will require a recovery downtime of at least a few weeks before you can get back to your normal regimen.
- No use of General Anesthesia. Anesthesia can interact with the medicine you take, creating complications of its own.
- Minimal risk of rejection. Since most stem cells used in therapy come from your own body, there’s theoretically less chance they will be rejected.
Surgery Leads to More Surgery
In some cases, surgery patients have to have repeat surgeries for years after the initial procedure.
Hip and knee replacement patients are among the highest risk groups, with as many as 1.6% of all patients having to undergo a repeat revision[25].
According to the last year’s data from the Canadian Institute of Health Information, hip and knee replacements cost patients almost $130 million per year[26], with the average cost of a repeat surgery being $13,700.
Other types of surgeries don’t lift the mood, either.
This 2014 study has found that 10% of the 120 with neck fracture patients[27] had to undergo a second surgery 2-24 months after the initial one
And, as this 2015 research has discovered, an increasing number of ACL[28] (anterior cruciate ligament) patients have to undergo a repeat surgery later on.
How Does Stem Cell Therapy Compare?
The two major differences between stem cell therapy and surgical intervention are:
- Stem cell therapy is a less invasive procedure. For this reason alone, many major complications are less common—including blood clots.
- Stem cell therapy empowers your own body’s ability to heal. Since the stem cells used are, for the most part, harvested from your own body.
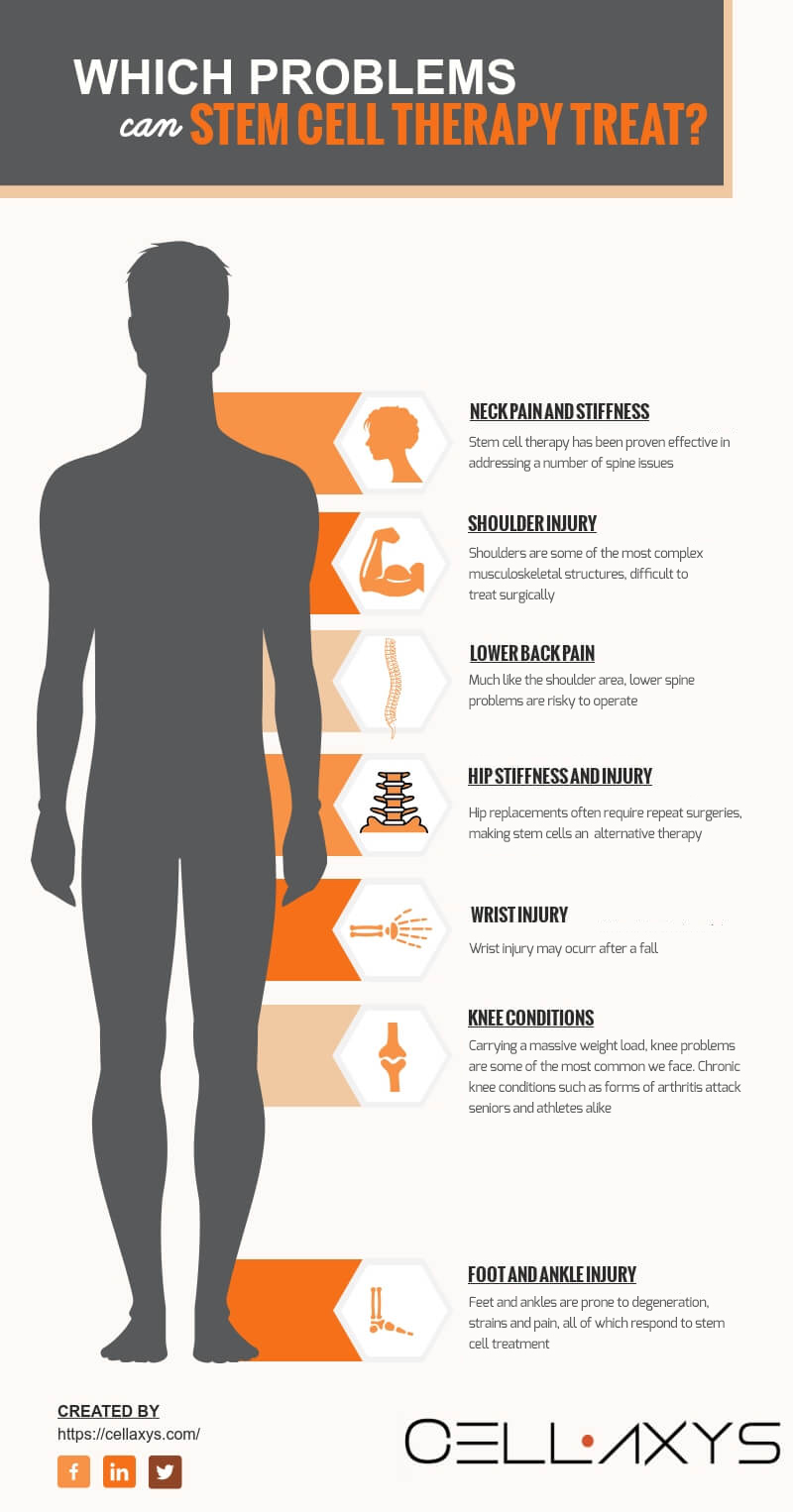
What Problems Can Stem Cell Therapy Treat?
Some people view stem cell therapy as a cure-all. Others view it as a supplementary alternative procedure that struggles to treat problems independently.
The truth lies in between.
Generally, there are two groups of conditions stem cell therapy can help with.
Stem Cell Therapy to Treat Blood and Immune System Diseases
What you need to know:
- Blood and immunodeficiency conditions are the oldest known problems stem cell therapy can solve
- Here at Cellaxys, we do not treat these types of conditions
- Common conditions include: leukemia, lymphoma, anemia
For 50 years following the first bone marrow transplant procedure, stem cell therapy was focused almost exclusively on blood and immunodeficiency disorders.
The main reason for this is simple: adult stem cells (harvested from your own body) have limited abilities to differentiate and multiply.
Meaning, the stem cells we knew about in the 1960s were enough to treat blood cancers and diseases, but not much else.
Since then, however, we have found many more sources of stem cells in our body, and we have learned their additional abilities to differentiate. This has lead to the expansion of stem cell therapy into the domain of orthopaedics.
Here at Cellaxys, we do not treat blood and immunodeficiency disorders with the help of stem cell therapy, thus we will not go into the details of the mechanics behind those treatments.
Stem Cell Therapy to Treat Orthopaedic and Spine Problems
What you need to know:
- Here at Cellaxys, we treat knee, spine, elbow, shoulder, wrist, hip, foot and ankle problems
- Stem cell therapy can be used to treat both acute injuries (trauma) and degenerative chronic conditions (e.g. osteoarthritis)
While the general dynamics of the therapy are the same for most patients, the reasons why they work in each individual case differ slightly:
Knee therapy. Issues and pain in the knee area are extremely common as our patient’s age. Reduced mobility and reoccurring pain affect their everyday life.
Knee Problems we treat:
- Commonly Treated Knee Pain Sources:
- Osteoarthritis
- Meniscus Tears
- PCL/ACL Partial Tears
- MCL & LCL Tears
- Cartilage damage and thinning
- Patellofemoral Pain
- Patella and Quadriceps Tendon Injuries
- Tendonitis
- Bursitis
- Inflammation
- Inflammation
- Reactive Arthritis: Rheumatoid, Gout related, etc
Elbow Problems. Being one of the most complex joints in the body, elbow injuries and conditions are extremely difficult to operate surgically, which makes stem cells a potential treatment option.
Elbow conditions treated:
- Lateral Epicondylitis, “Tennis Elbow”
- Medial Epicondylitis. “Golfers Elbow”
- Arthritis
- Articular Cartilage thinning or injury (“OCD” lesions)
- UCL injuries “Tommy John’s”
- Triceps Tendon injury or tear
Shoulder Problems. An intersection of several joints that combine tendons, ligaments, and muscles, the shoulders are responsible for an incredible range of motion.
Shoulder conditions treated:
- Rotator Cuff Tendon inflammation and tears
- Arthritis
- Labrum Tears
- AC Joint pain, instability, and arthritis
- Shoulder instability
- Biceps Tendon injuries
- Non-Union Fractures
- Post-surgical pain or healing compliment
Hip Problems. There are two distinctive types of pain in the hip: pain inside the hips or groin area usually indicates joint problems; pain that radiates towards the outside of the hips is likely caused by a strained muscle.
Hip conditions treated:
- Arthritis (rheumatoid arthritis and osteoarthritis are particularly common in the hip area)
- Cartilage damage
- Labrum Tears
- Trochanteric Bursitis
- Gluteus Medius and Minimus tendonitis or Partial Tears
- Pain from FAI (Femoral Acetabulum Impingement)
- Post surgical pain or healing compliment
Neck therapy. Neck injuries and natural wear-and-tear usually go unnoticed for long periods of time, since there’s no usual pain right after trauma or injury. However, they could be a part of a larger upper spine problem.
Neck conditions treated:
- Cervical spine wear-and-tear (cervical arthropathy usually arthritis worsens with age, causing severe chronic pain and stiffness in the neck)
- Ankylosing spondylitis (an aggressive form of arthritis that attacks your spinal bones if affecting facet joints)
- Sprains and strains (soft tissues around the spinal joints are subject to overstretching and tear)
Lower back therapy. Due to its interconnection with the nervous system, lower spine issues can be—quite literally—paralyzing.
Lower back conditions treated:
- Degenerative disc disease (spongy tissue of cartilage between the spinal discs that may breakdown and cause pain)
- Spinal stenosis (certain types of stenosis caused by osteoarthritis)
Can Anyone Get Stem Cell Therapy?
What you need to know:
- Most surgery candidates are potentially good stem cell therapy candidates
- We review all of the patient’s data before making a recommendation
Readers who have made it to this section will expect to see long lists of criteria and health factors, all of which would require a checkmark to make them eligible for stem cell treatment.
They’re not to blame. After all, most surgical procedures have a long list of “eligibility criteria.”
With stem cells, it’s different. Due to their naturally regenerative, minimally invasive nature, most patients could be a good candidates for stem cell therapy treatment.
We choose our candidates by asking ourselves:
- Can stem cell therapy help this particular patient with this particular issue?
- Can other alternatives (surgery, physical therapy) be more effective in this particular case?
We do this by evaluating a number of criteria:
- The scope of the injury or condition
- The nature of the injury or condition
- Patient’s medical history
- Patient’s experience with other treatment methods
- Patient’s health condition, strength, and range of motion
- X-ray, CT, or MRI imaging information
After reviewing all this data, our lead physicians make a medical decision on whether stem cell therapy would be effective.
Want to activate your body’s natural ability to heal itself?
Consider Stem Cell Therapy.
Fill out the form below to request your FREE consultation
Part II: Does Stem Cell Therapy Work?
If you’re just learning about stem cells now, you’re probably skeptical about whether they actually work, and how much of a change can they actually produce for patients.
We’ll give you information from three sources to form an opinion of your own:
- Medical research
- Professional world-class athlete cases
- Our own patient stories
Stem Cell Results in Medical Research
Study 1[29]: “Osteoarthritis and stem cell therapy in humans: a systematic review” (June 2018)
Problem treated: Osteoarthritis
Number of patients: 2,390
Nature of stem cells: Adipose (fat) tissue [50% of cases] ; bone marrow [50% of cases]
Results: Stem cell therapy had a positive effect on osteoarthritis patients
Study 2[30]: “Cell-Based Therapies for Lumbar Discogenic Low Back Pain” (January 2018)
Problem treated: Low back pain
Number of patients: –
Nature of stem cells: Bone marrow
Results: Stem cell therapy significantly reduced low back pain for all patient groups
Study 3[31]: “Stem cells – biological update and cell therapy progress” (May 2017)
Problem treated: Spinal cord injury (SCI)
Number of patients: 377
Nature of stem cells: –
Results: Stem cell therapy is a safe and efficient SCI treatment, improving sensory and bladder functions
Study 4[32]: “Stem cell therapy for diabetic foot ulcers: a review of preclinical and clinical research” (July 2018)
Problem treated: Diabetic foot ulcers (DFU)
Number of studies involved: 89
Nature of stem cells: –
Results:
- Stem cell therapy is an effective treatment method for diabetic foot ulcers patients
- Stem cell therapy is a good alternative to amputation
Study 5[33]: “Biologic augmentation of rotator cuff repair with mesenchymal stem cells during arthroscopy improves healing and prevents further tears: a case-controlled study” (September 2014)
Problem treated: Rotator cuff repair; re-tear rates go as high as 90
Number of patients: 90
Nature of stem cells: Bone marrow
Results: 100% of rotator cuff repairs stayed intact 6 months after the procedure for stem cell patients, compared to 67% of the control group.
There are many other studies, most of which arrive at similar conclusions:
- Stem cells provide a positive effect in most orthopedic cases
- Stem cells complications are typically rare
Stem cells are not the cure-all for any patient, but they do help tremendously in the right situations.
Stem Cell Results in Professional Athletics
A number of high-profile sports stars have undergone the procedure.
Rafael Nadal: Stem Cell Treatment for Spine
In 2014, one of the world’s most decorated tennis players, Rafael Nadal, underwent stem cell therapy[34].
The problem they were to treat was a common one for tennis players: a back injury, caused by deteriorating cartilage around one of his lower spine joints.
The treatment took place over the course of 5 weeks, which enabled Nadal to keep leading positions in the world’s tennis scene.
The therapy was so successful that Nadal underwent a second treatment soon after for a knee injury.
Pau Gasol: Stem Cell Therapy for Knees
The 2013 season was defined by traumas and missed games for one of the NBA’s best power forwards, Pau Gasol.
The degenerating cartilage tissue around the athlete’s knees was limiting the veteran athlete to the bench[35]. The problems were causing severe pain and stopped the player from moving freely around the court.
Gasol underwent an autologous stem cell transplantation the same year. The treatment was aimed at restoring the degenerative tissue and stimulate growth.
Peyton Manning: Stem Cell Treatment for Neck
Peyton Manning, the legendary quarterback for the Indianapolis Colts, was the original case study in stem cell therapy for athletes.
The football superstar was suffering from a bulging disk[36], which caused severe neck pain and restricted mobility.
Manning turned to stem cell specialist in Europe, where adipose (fat) tissue stem cells had been harvested from the athlete and administered into the problematic area. The main focus was on regenerating damaged nerve tissue around the area.
Before that, Peyton Manning had undergone surgical treatment several times, to little effect.
The therapy proved successful and allowed the quarterback to return to the game, setting new standards for injury and chronic condition therapy in professional sports.
Cristiano Ronaldo: Stem Cell Therapy for Knees
After an unsuccessful fall during the 2016 match versus Villarreal, CT scans showed that the problem was more than a muscle spasm: it was a torn cartilage.
Ronaldo turned to stem cell therapy[37] to avoid the risk associated with surgical intervention.
Reportedly, part of the reason why the soccer superstar turned to alternative treatments was the fact that he “lost all faith” in the medical staff at Santiago Bernabeu, his home stadium.
Stem Cell Results In Our Own Patients
Visit stories of a few of our patients.
Disclaimer: results may vary from patient to patient. Please contact us to get a detailed explanation.
Bryan Plaster, 40 Years Old: From Crashing Into a Tree to Running 40 Miles a Day
Problem treated: Knee injury
Cause of the problem: Snowboarding accident
Nature of stem cells: Bone marrow and adipose (fat) tissue
Results: The tear was resolved completely; the damaged fibers restored fully
Joey Varner, 40 Years Old: Shoulder and Hip Arthritis, Rotator Cuff Tendonitis Treated

Problem treated: Shoulder and hip arthritis, rotator cuff tendonitis
Cause of the problem: Mechanical wear and tear from years of contact (martial arts) sports. Several surgeries didn’t resolve the issue, causing stiffness and pain
Nature of stem cells: Adipose (fat) tissue
Results: Almost 100% restored range of motion in hip and shoulder; 100% reduction in pain
Bob Kendzior, Senior: From Chronic Arthritis and Injury to Normal Everyday Life
Problem treated: Arthritic condition in both knees; shoulder and hip injury
Cause of the problem: Mechanical wear and tear, sudden trauma
Nature of stem cells: Adipose (fat) tissue
Results: Bob is back to normal life; he likes to “run, walk, bicycle, golf and run”
Want to activate your body’s natural ability to heal itself?
Consider Stem Cell Therapy.
Fill out the form below to request your FREE consultation
Part III: How to Prepare for Stem Cell Therapy?
When it comes to stem cell preparation, there are a few things you could do that could actually help us maximize the therapy results.
However, it’s important to note that proper recovery (discussed in Part IV) is much more important for the final results of your treatment.
Stem cells need a healthy environment to develop and grow.
Nevertheless, here’s what you can do before the procedure to make the whole process smoother and more effective:
To-do #1: Cut Down Calories
Reducing the amount of calories taken—even for a short period of time—has been shown to positively affect the number of stem cells[43] in your body circulation.
The more stem cells you have, naturally, the easier it is to harvest a needed amount of them for the treatment, which will increase your chances of a successful recovery.
Another study has shown that short-term calorie reduction enhances skeletal muscle stem cell function[44], too. The study also concluded that short-term calorie reduction improves muscle regeneration and “enhances stem cell transplant efficiency.”
In 2014, a group of scientist also found that calorie restriction is strongly linked to slower aging[45] of our stem cells, “prolonging the capacity of stem cells to self-renew, proliferate, differentiate, and replace cells in several adult tissues.”
After all, there’s a reason why low-calorie Japanese communities live the longest, healthiest lives[46].
To-do #2: Cut Sugar
Related to the previous point, sugar restriction deserves a separate point of its own.
The most important reason why we suggest cutting down on sugar is because there is evidence that high sugar levels may cause several adverse effects[47] on the therapy, which basically means that your procedure will be less effective, or the change will take longer to manifest.
In general, cutting sugar is always a good idea, as it stimulates a more healthy lifestyle, which is the cornerstone of a successful stem cell treatment—both before and after the actual procedure.
To-do #3: Exercise
Exercise is actually both scientifically and practically proven to increase stem cell activity, which is a big advantage going into the therapy.
This 2017 study[48] found that “for skeletal muscle, the effect of physical exercise is becoming more and more clear”, which could be summarized in simple terms as stem cell activation. Which means that stem cells function better and multiply faster, given physical exercise stimulation.
Another 2009 study has shown that strenuous exercise has significantly increased[49] the number of stem cells in circulation.
It has even been shown in professional athletes that intense exercise can help cells migrate[50] better from bone marrow into the circulation, improving their quantity and function.
What is the proper exercise to activate your stem cells?
To put it briefly, it doesn’t matter what you do exactly as long as you’re taking your muscles to exhaustion. Whether it’s high repetitions with low weights, or few repetitions with heavy weights, the important thing is to exhaust the muscle. (As long as you’re doing everything with correct form, of course.)
Other (Non) Tips
You’ll find many tips online that may or may not be true. Some of them will be too vague to prove useful, while others will be specific but incorrect.
The three tips we’ve outlined so far—we’ve witnessed their effects ourselves. However, there are very few peer-reviewed pre-procedural protocols that have been properly researched.
So, the next time you come across tips like these, use a healthy dose of skepticism:
- Go on a high-altitude vacation. We’ve seen this quoted on several occasions on the internet. The argument is that lower oxygen levels improve the function of stem cells. We would advise not to follow this point blindly, because there are other mechanics at play that could “cancel out” the effects of lower oxygen.
- Stop taking over-the-counter medications. The other thing we see often is a definite list of all the supplements and medications that “all” patients should avoid taking. In reality, each case is different, and which medications and supplements could interact with the treatment depend on a number of factors, including the patient’s age, nature of the injury, type of stem cells used, and a number of other criteria. Always consult with your physician before making a decision to start/stop taking any supplements or medications.
Part IV: How To Maximize Stem Cell Results After the Treatment (Recovery and Guidelines)
Stem cells multiply and differentiate within your body naturally.
Therefore, in order to achieve best possible results, we need to create a healthy environment for the stem cells to thrive. We can do that by:
- Cutting down on harmful habits
- Exercising regularly and staying active
- Eating a healthy diet
Here is your approximate activity guideline and recovery timeline for the next few months:
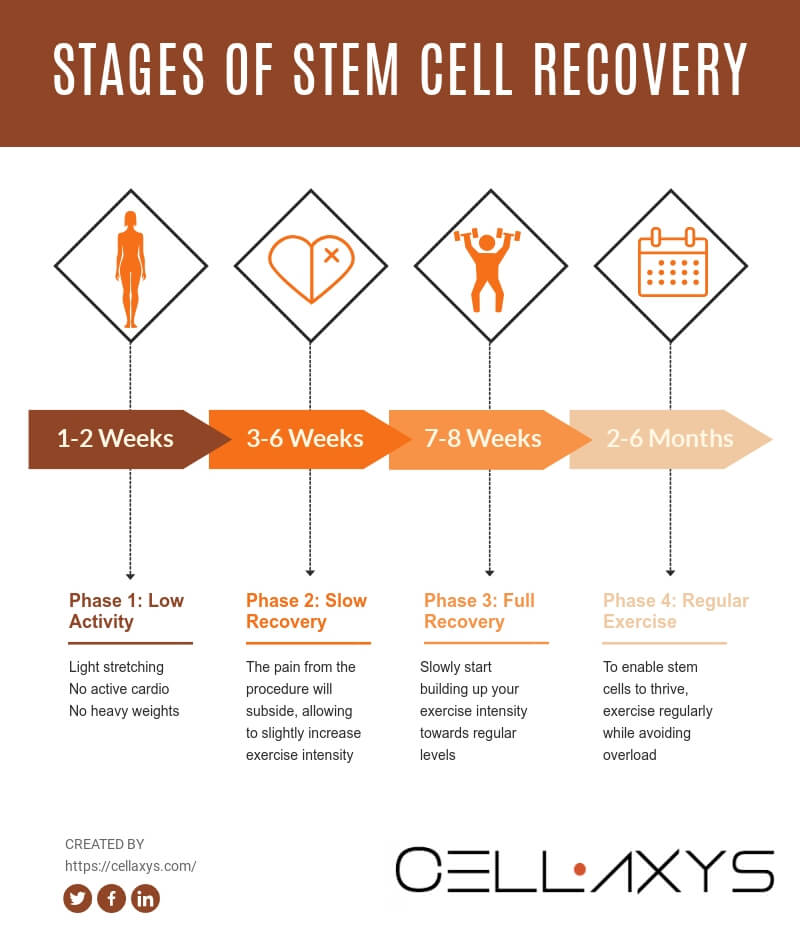
Week 1-2: Light Exercise and Mild Activity
During the first two weeks, moderation is key. You do not want to overload your body as it can cause another injury while your body is experiencing during this vulnerable period of inner transformation.
At this time, the stem cells are just starting to form and differentiate within your body, therefore overstretching and overloading your joints can be dangerous and reverse the effects of the therapy, if not make them outright worse.
Be extremely cautious to put pressure on the joints near the treatment area.
Here are a few important guidelines for weeks 1 and 2:
- Avoid lifting more than 10 pounds of weight at once
- Avoid walking up long flights of stairs
- Avoid intense stretching
- Avoid intense cardio exercise and active sports
However, it is absolutely crucial that you do not start off your recovery in a fully sedentary manner. Your body needs the oxygen and active stimulation to continue to grow and develop the stem cells.
Even though you might feel some mild pain and discomfort in the treatment area, do not give in to the natural instinct of laying in your bed for two weeks.
Staying active is extremely important during the recovery phase to achieve optimal results. In fact, prolonged inactivity after your stem cell treatment can dramatically reduce results.
Recommended exercises during this period:
- Light yoga, stretching, pilates
- Lifting weights (20-30% of your normal weight load)
- No running or outdoor sports
Week 3-6: Walking, Swimming, Light Lifting, but No Running
Weeks 3 and 4 are typically when patients stop feeling any pain after the procedure.
For that reason, it is also the period when most patients injure themselves by overstretching or putting too much pressure on the musculoskeletal systems.
During this period, everything applies that was said about weeks 1 and 2, except:
- You can now increase your stretch intensity a little
- Weight lifting can now be safe up to 50% of your normal weight load
- Active walking and swimming can now be resumed
- Running is still strongly not recommended
Week 7-8: Slowly Progressing Back to Normal Exercise
“Active but cautious” is still the name of the game during weeks 7-8.
However, as your body continues to get stronger, you can slowly start raising your workout intensity to your normal levels. Always listen to your body as you increase the workload.
Month 2-6: Regular Exercise Without Sudden Changes
This period of a few months is crucial for the success of your stem cell therapy.
The most important thing during this period is to stay active and exercise regularly, but at the same time to not increase your workload or change your exercise plan suddenly.
For example, some bodybuilding enthusiasts and high-intensity athletes tend to often switch things up in their workout routine, in order to “keep their muscles guessing.” This way, hypertrophy and other favorable body reactions are stimulated.
While this might make sense for an entirely healthy individual for a period of time, it’s best to keep things simple and consistent during your recovery phase.
Part V: Questions People Ask, Answered
1. Are stem cell procedures covered by insurance? Are they covered by Medicare?
Currently in the US and many other westernized countries, only stem cell therapies designed to treat blood and bone marrow diseases—such as leukemia and lymphoma—can be fully or partially reimbursed by insurance and Medicare.
Therapies aimed to help patients avoid surgery after an injury or when suffering from a chronic condition are still mostly considered “experimental” and are usually not covered by insurance or Medicare; however, exceptions do happen on a case-by-case basis.
2. Is stem cell therapy legal?
Yes.
The usage of adult (bone marrow and adipose tissue) and umbilical cord stem cells to treat various conditions and diseases is perfectly legal[10].
The only stem cells that are prohibited in therapy and are highly regulated in research are embryonic stem cells.
3. Is stem cell therapy FDA-approved?
FDA allows for “minimal manipulation”[12] to happen during the transplantation phase. Here is what “minimal manipulation” means:
- The processing of the tissue does not alter its original characteristics
- The processing does not alter any biological characteristics of cells and tissue
4. Is stem cell therapy ethical?
As we’ve mentioned previously, there is a lot of controversy surrounding stem cell therapy.
However, the controversy is mainly sparked by embryonic stem cells, which are not used in practical therapy. It is not legal to use embryonic stem cells in therapy within the US.
Umbilical cord stem cells are donated by informed consent by a newborn’s parents for research and medical purposes. The transfer of these stem cells to therapy clinics is a highly controlled process.
Other sources—your own bone marrow or adipose (fat) tissue stem cells—shouldn’t raise any ethical questions as they are part of your body.
5. Can stem cell therapy cure diabetes?
The potential of stem cells is as powerful as it is exciting. There is important ongoing research in the possible application of stem cell therapy in curing a number of previously unchallenged diseases, including diabetes[51]. As we do not provide this type of treatment, we will refrain from further comment.
6. Are stem cell injections painful?
This is a question we get quite a lot. The injection itself is no more painful than your typical shot at the doctor’s office. For a couple of weeks after the procedure, however, you might feel mild pain in the area, which is completely normal and shouldn’t interrupt your daily activities or light exercise.
7. How long does it take for stem cell therapy to work?
It takes a few weeks to a few months for stem cells to start actively multiplying and differentiating within the patient’s body. Most of our patients feel significant results within 2-6 months period.
Want to activate your body’s natural ability to heal itself?
Consider Stem Cell Therapy.
Fill out the form below to request your FREE consultation
References
1.“Researchers Clarify the Identity of Stem Cells” by University of Calgary. Source:https://medicalxpress.com/news/2018-05-identity-brain-stem-cells.html
2.”Bone Marrow Diseases” by U.S. National Library of Medicine. Source: https://medlineplus.gov/bonemarrowdiseases.html
3.”NCI Dictionary of Cancer Terms” by National Cancer Institute. Source: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/blood-stem-cell
4.”Muscle Stem Cells” by Nature. Source: https://www.nature.com/subjects/muscle-stem-cells
5.”Stem Cells: Where Do They Live and What They Can Do?” by EuroStemCell. Source: https://www.eurostemcell.org/skin-stem-cells-where-do-they-live-and-what-can-they-do
6.”Liver Stem Cells” by Matthews VB, Yeoh GC. Source: https://www.ncbi.nlm.nih.gov/pubmed/16118112
7.”Regeneration in Humans” by Wikipedia. Source: https://en.wikipedia.org/wiki/Regeneration_in_humans#Naturally_regenerating_appendages_and_organs
8.”Stem Cells in the Umbilical Cord” by Mark L. Weiss, Deryl L. Troyer. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3753204/
9.”Stem Cell Information” by National Institutes of Health. Source: https://stemcells.nih.gov/info/basics
10.”Stem Cell Laws” by Wikipedia. Source: https://en.wikipedia.org/wiki/Stem_cell_laws#United_States
11.”First Person Treated in Milestone Stem Cell Trial” by Andy Coghlan. Source: https://www.newscientist.com/article/dn19570-first-person-treated-in-milestone-stem-cell-trial
12.”Regulatory Considerations for Human Cells, Tissues, and Cellular and TissueBased Products: Minimal Manipulation and Homologous Use” by Food and Drug Administration. Source: link
13.”After Surgery: Discomforts and Complications” by University of Rochester. Source: https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=85&ContentID=P01390
14.”What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients” by Beswick AD, Wylde V, Gooberman-Hill R, et al. Source: https://bmjopen.bmj.com/content/2/1/e000435
15.”Many diseases increase the risks of hip fracture surgery” by University of Eastern Finland. Source: https://www.sciencedaily.com/releases/2018/11/181130111645.htm
16.”Complications of total hip arthroplasty” by Greg A Erens, MD. Source: https://www.uptodate.com/contents/complications-of-total-hip-arthroplasty
17.Reis RC, de Oliveira MF, Rotta JM, Botelho RV. Risk of complications in spine surgery: a prospective study. Open Orthop J. 2015;9:20-5. Published 2015 Jan 31. doi:10.2174/1874325001509010020. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4321205/
18.Proietti L, Scaramuzzo L, Schiro’ GR, Sessa S, Logroscino CA. Complications in lumbar spine surgery: A retrospective analysis. Indian J Orthop. 2013;47(4):340-5. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3745686/
19.Kroslak, M., & Murrell, G. A. C. (2018). Surgical Treatment of Lateral Epicondylitis: A Prospective, Randomized, Double-Blinded, Placebo-Controlled Clinical Trial. The American Journal of Sports Medicine, 46(5), 1106–1113. Source: https://journals.sagepub.com/doi/abs/10.1177/0363546517753385
20.Hackl M, Beyer F, Wegmann K, Leschinger T, Burkhart KJ, Müller LP. The treatment of simple elbow dislocation in adults. Dtsch Arztebl Int. 2015;112(18):311-9. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4455254/
21.Backhouse MR, Vinall-Collier KA, Redmond AC, Helliwell PS, Keenan AM. Interpreting outcome following foot surgery in people with rheumatoid arthritis. J Foot Ankle Res. 2016;9:20. Published 2016 Jul 8. doi:10.1186/s13047-016-0153-6. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4938997/
22.Chou LB, Wagner D, Witten DM, et al. Postoperative pain following foot and ankle surgery: a prospective study. Foot Ankle Int. 2008;29(11):1063-8. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2743476/
23.Kise Nina Jullum, Risberg May Arna, Stensrud Silje, Ranstam Jonas, Engebretsen Lars, Roos Ewa M et al. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up BMJ 2016; 354 :i3740. Source: https://www.bmj.com/content/354/bmj.i3740
24.Beaufils P, Becker R, Kopf S, Matthieu O, Pujol N. The knee meniscus: management of traumatic tears and degenerative lesions. EFORT Open Rev. 2017;2(5):195-203. Published 2017 May 11. doi:10.1302/2058-5241.2.160056. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5489759/
25.”New hip and knee replacements ‘more likely to need repeat surgery” by Kate Devlin. Source: https://www.telegraph.co.uk/news/uknews/2663548/New-hip-and-knee-replacements-more-likely-to-need-repeat-surgery.html
26.”Repeat hip and knee replacements cost $130 million annually” by Canadian Institute for Health Information. Source: https://www.cihi.ca/en/repeat-hip-and-knee-replacements-cost-130-million-annually
27.Kain MS, Marcantonio AJ, Iorio R. Revision surgery occurs frequently after percutaneous fixation of stable femoral neck fractures in elderly patients. Clin Orthop Relat Res. 2014;472(12):4010-4. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4397802/
28.”Many young ACL surgery patients need second surgery later on” by Hospital for Special Surgery. Source: https://www.sciencedaily.com/releases/2015/05/150501103455.htm
29.”Osteoarthritis and stem cell therapy in humans: a systematic review” by Jevotovsky DS, Alfonso AR, Einhorn TA, Chiu ES. Source: https://www.ncbi.nlm.nih.gov/pubmed/29544858
30.Cell-Based Therapies for Lumbar Discogenic Low Back Pain: Systematic Review and Single-Arm Meta-analysis. Wu T, Song HX, Dong Y, Li JH. Spine (Phila Pa 1976). 2018 Jan 1;43(1):49-57. doi: 10.1097/BRS.0000000000001549. Source: https://www.ncbi.nlm.nih.gov/pubmed/26953666
31.Fan X, Wang JZ, Lin XM, Zhang L. Stem cell transplantation for spinal cord injury: a meta-analysis of treatment effectiveness and safety. Neural Regen Res. 2017;12(5):815-825. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5461621/
32.Lopes L, Setia O, Aurshina A, Liu S, Hu H, Isaji T, Liu H, Wang T, Ono S, Guo
X, Yatsula B, Guo J, Gu Y, Navarro T, Dardik A. Stem cell therapy for diabetic
foot ulcers: a review of preclinical and clinical research. Stem Cell Res Ther.
2018 Jul 11;9(1):188. doi: 10.1186/s13287-018-0938-6. PubMed PMID: 29996912;
PubMed Central PMCID: PMC6042254. Source: https://www.ncbi.nlm.nih.gov/pubmed/29996912
33.Hernigou P, Flouzat Lachaniette CH, Delambre J, Zilber S, Duffiet P,
Chevallier N, Rouard H. Biologic augmentation of rotator cuff repair with
mesenchymal stem cells during arthroscopy improves healing and prevents further
tears: a case-controlled study. Int Orthop. 2014 Sep;38(9):1811-8. doi:
10.1007/s00264-014-2391-1. Epub 2014 Jun 7. PubMed PMID: 24913770. Source: https://www.ncbi.nlm.nih.gov/pubmed/24913770
34.”Rafael Nadal to undergo stem-cell treatments on his injured back” by Matt Bonesteel. Source: https://www.washingtonpost.com/news/early-lead/wp/2014/11/10/rafael-nadal-to-undergo-stem-cell-treatments-on-his-injured-back/?utm_term=.c3e7dbd2f4c7
35.”Pau Gasol has knee procedure, to receive stem cell injections” by Eric Pincus. Source: https://www.latimes.com/sports/lakers/lakersnow/la-sp-ln-lakers-pau-gasol-knee-procedure-20130509-story.html
36.”Peyton Manning Underwent Stem Cell Treatment For Neck Injury” by Amanda L. Chan. Source: https://www.huffpost.com/entry/peyton-manning-stem-cell-treatment_n_970763
37.”Cristiano Ronaldo will undergo stem cell treatment as Real Madrid star races to be fit to face Manchester City in second-leg clash” by Oliver Todd. Source: https://www.dailymail.co.uk/sport/football/article-3562460/Cristiano-Ronaldo-undergo-stem-cell-treatment-Real-Madrid-star-races-fit-face-Manchester-City-second-leg-clash.html
38.”What Is This Knee Treatment Kobe Bryant Goes All the Way to Germany For?” by Will Carroll. Source: https://bleacherreport.com/articles/1798763-what-is-this-knee-treatment-kobe-bryant-goes-all-the-way-to-germany-for
39.”PRP Therapy Helps Tiger Woods Recover” by Cedar Stem Cell Institute. Source: https://www.cedarsci.com/blog/prp-therapy-tiger-woods/
40.”PRP, stem cell and Warriors G Steph Curry’s quick return from knee injury” by John Canzano. Source: https://www.oregonlive.com/sports/oregonian/john_canzano/2016/04/steph_currys_return_from_mcl_s.html
41.”STEM CELL THERAPY PLAYS A CRUCIAL ROLE FOR ATHLETES IN THE 2012 OLYMPIC GAMES: KOBE BRYANT, DARA TORRES AND DAVID PAYNE” by Metro MD. Source: https://www.metro-md.com/stem-cell-therapy-plays-a-crucial-role-for-athletes-in-the-2012-olympic-games-kobe-bryant-dara-torres-and-david-payne/
42.”Green’s stem-cell success story bodes well for Manning” by Albert Breer. Source: http://www.nfl.com/news/story/09000d5d8227e0ce/article/greens-stemcell-success-story-bodes-well-for-manning
43.Mikirova NA, Casciari JJ, Hunninghake RE, Beezley MM. Effect of weight
reduction on cardiovascular risk factors and CD34-positive cells in circulation.
Int J Med Sci. 2011;8(6):445-52. Epub 2011 Aug 1. PubMed PMID: 21850193; PubMed
Central PMCID: PMC3156990. Source: https://www.ncbi.nlm.nih.gov/pubmed/21850193
44.Cerletti M, Jang YC, Finley LW, Haigis MC, Wagers AJ. Short-term calorie restriction enhances skeletal muscle stem cell function. Cell Stem Cell. 2012;10(5):515-9. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3561899/
45.Mazzoccoli G, Tevy MF, Borghesan M, Delle Vergini MR, Vinciguerra M. Caloric
restriction and aging stem cells: the stick and the carrot? Exp Gerontol. 2014
Feb;50:137-48. doi: 10.1016/j.exger.2013.10.014. Epub 2013 Nov 6. Review. PubMed
PMID: 24211426. Source: https://www.ncbi.nlm.nih.gov/pubmed/24211426
46.”The Okinawa diet – could it help you live to 100?” by Michael Booth. Source: https://www.theguardian.com/lifeandstyle/2013/jun/19/japanese-diet-live-to-100
47.Saki N, Jalalifar MA, Soleimani M, Hajizamani S, Rahim F. Adverse effect of high glucose concentration on stem cell therapy. Int J Hematol Oncol Stem Cell Res. 2013;7(3):34-40. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3913149/
48.Ceccarelli G, Benedetti L, Arcari ML, Carubbi C, Galli D. Muscle Stem Cell and Physical Activity: What Point is the Debate at?. Open Med (Wars). 2017;12:144-156. Published 2017 Jul 24. doi:10.1515/med-2017-0022. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5529938/
49.Möbius-Winkler S, Hilberg T, Menzel K, Golla E, Burman A, Schuler G, Adams V.
Time-dependent mobilization of circulating progenitor cells during strenuous
exercise in healthy individuals. J Appl Physiol (1985). 2009 Dec;107(6):1943-50.
doi: 10.1152/japplphysiol.00532.2009. Epub 2009 Oct 1. PubMed PMID: 19797690. Source: https://www.ncbi.nlm.nih.gov/pubmed/19797690
50.Schmidt A, Bierwirth S, Weber S, Platen P, Schinköthe T, Bloch W. Short
intensive exercise increases the migratory activity of mesenchymal stem cells. Br
J Sports Med. 2009 Mar;43(3):195-8. Epub 2007 Dec 10. PubMed PMID: 18070806. Source: https://www.ncbi.nlm.nih.gov/pubmed/18070806
51.”Stories of Hope: A Stem Cell Therapy for Diabetes” by California’s Stem Cell Agency. Source: https://www.cirm.ca.gov/our-progress/stories-hope-stem-cell-therapy-diabetes
52. Miana VV, González EAP. Adipose tissue stem cells in regenerative medicine. Ecancermedicalscience. 2018;12:822. Published 2018 Mar 28. doi:10.3332/ecancer.2018.822. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5880231/
53. “FDA announces comprehensive regenerative medicine policy framework” by Food and Drug Administration. Source: https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm585345.htm




