Published on: December 18, 2019 | Updated on: November 3, 2024
The meniscus is a soft tissue patch in the knee. Due to its location in the body and load-bearing capacity, these vital tissues can become damaged over time.
Depending on the severity of the issue, you may have to undergo surgery to fix it. While surgeries can help return a knee to normal function, they may take a long time to recover.
This makes us wonder, “How long is the meniscus tear surgery recovery time?” Let’s find out.
Do you have Meniscus pain?
Fill out the form below to schedule your FREE virtual consultation
Anatomy of the Meniscus
Two menisci, oval-shaped cartilage disks wedged between the upper leg (thigh bone/femur) and lower leg (shin bone/tibia) make up the knee joint. One of these disks rests on the knee joint’s inner (medial) side, and the other sits on the outer (lateral) side. The patella (knee cap) is positioned at the front of the knee and slightly above both the menisci.
Together, these disks act as shock absorbers, minimizing the stress our knees face from the constant pressure we place on them. Most importantly, the menisci help ensure that the articular cartilage that coats the bones stays intact, for if this thin layer of cartilage degrades, pain, instability, and other symptoms may occur.
In addition to these protective elements, the menisci improve the knee’s stability. Their placement on either side of the knee joint prevents awkward motions outside the normal range of knee movement. In a way, they act like blocks you might place behind a tire to stop a car from slipping out of place.
When a meniscal tear occurs, whether due to acute knee injury or simple age-related degeneration, it usually leads to a range of problems.
- Pain, especially when the knee bears weight or the outer knee is touched
- Swelling
- Popping and clicking sensations
- Reduced range of motion
- Knee locking or “catching”
- Knee instability
As the meniscal tear worsens, the symptoms will become chronic. Unfortunately, meniscal tears cannot fully heal independently or with conservative (non-invasive) treatment. Thus, one option many turn to once a meniscal tear is diagnosed is surgical intervention.
Before surgery, a doctor must fully qualify and diagnose a person’s meniscal tear.
Meniscus Tear Diagnosis
Patients who believe they would benefit from surgery for their meniscus tear must first approach their symptoms conservatively. Depending on the severity of the tear, over-the-counter medication and physical therapy may be recommended for first-round treatments.
If these fail to restore function or reduce symptoms, doctors will move on to a second, more extensive diagnostic procedure before recommending the patient for surgery.
Physical exam and medical history
Before any doctor-sponsored intervention takes place, a physical exam and medical history report must be prepared. The doctor will talk to the patient about their symptoms and review past medical reports to reduce the probability that other conditions may be causing them.
The doctor will examine the knee, test the limits of its inner and outer range of motion, and palpate (apply pressure) around it. They may also rotate the knee or ask the patient to stand on the affected leg while turning their body.
If these tests are positive and medical history indicates an issue, doctors will proceed to medical imaging to get a side view of the knee joint and its structures.
Imaging tests
Imaging tests are ordered to confirm the suspicion of a meniscal tear. These include:
- X-ray: While these tests do not show the meniscus, they will be used to identify issues with the knee bones and determine if another problem, such as osteoarthritis, is linked to the patient’s pain.
- MRI: Using magnetic fields and image-capturing devices, doctors can examine the health of the soft tissues within the knee with an MRI. While these tests are helpful, they may be unreliable, as certain structures within the knee may resemble a meniscus tear. Using MRIs in addition to other tests listed here will help ensure that a meniscus tear is, in fact, the issue.
- Ultrasound: These tests map the knee’s soft and hard structures using sound waves. Doctors can determine if soft tissues are in their proper location or if some may be getting caught in the knee joint during movement.
- Arthroscopy: The most invasive of these tests, but by far the most accurate. Suppose doctors cannot determine the state of the meniscus using the above-mentioned conservative imaging techniques. In that case, they will create an incision in the knee and place a small camera within the incision. This technique gives doctors a crystal-clear image of the meniscus condition and will eliminate any other probable cause.
Surgical intervention is ultimately the last option, with other possibilities eliminated and conservative treatments failed. While many patients opt for this treatment, quite a few come into surgery unprepared for what to expect.
Research and ask a healthcare professional before applying surgical intervention to a health issue
Factors Influencing Recovery Time
The time it takes to recover from the surgery depends on several factors. Understanding these will help set accurate expectations and determine how soon you can return to your everyday routine and work.
Type of Surgery
Two types of surgeries are performed in the category of meniscus surgery, which determines how soon you will recover. There is a partial meniscectomy, which removes the damaged portion of the meniscus. It is less invasive than complete meniscus repair and faster to recover from.
The long-term effects, though, could be a higher risk of arthritis due to the reduced cushioning ability of the meniscus.
It usually takes 4-6 weeks for people to recover from the surgery and resume their daily activities.
In complete meniscus repair surgery, the torn meniscus is stitched up so it can heal. This strategy preserves the meniscus and also prevents the joint’s degeneration. However, the recovery timeline is longer, and the tissue may take 3-6 months to heal.
Age and Health
Young individuals and patients who do not have major health issues recover faster than older patients. Our body’s ability to heal naturally decreases as we age, so the healing process is longer. People with health conditions like obesity, diabetes, and arthritis or who are over the age of 60 have longer healing times.
Physical Activity
People who are physically active before the surgery can recover faster. The better your shape and fit, the quicker and easier it is for you to return to physical activities and work.
Meniscus Tear Surgery Recovery Timeline
Surgery for meniscal tears is minimally invasive, though recovery times can be surprisingly long. Additionally, while specific symptoms are often reduced, overall success is highly subjective to the individual patient.
Despite these concerns, many patients still opt for surgery. Patients should be as prepared as possible to ensure the highest degree of success. Below, we’ve outlined some critical points in the surgical process and what to expect once the surgical intervention occurs.
Be sure to talk to your doctor about any concerns and questions you raise while studying the following notes.
- Preparing for Meniscus Tear Surgery: Successful surgeries begin with adequate preparation. These preliminary steps help ensure patient safety and may be critical in determining the outcome of the meniscus repair surgery.
- Schedule bloodwork to reduce outside risks such as aversion to anesthetics or uncovering unknown blood or autoimmune disorders.
- Arrange for a ride to and from the hospital. Patients undergoing meniscus tear surgery will be prescribed medications that may prevent them from driving; it is best to have options when going to and from the hospital.
- Prepare a small luggage parcel for about two or three days’ worth of trip. Toiletries, entertainment, and clothes may be necessary for the hospital stay.
- Follow your doctor’s order entirely. Suppose they give a timeline for refraining from eating or drinking. In that case, it is essential to follow these guidelines, as anesthetics may interfere with the body’s natural digestive processes, leading to complications during surgery.
- Maintaining an adequate sleep schedule can help boost the body’s resilience to post-surgical pain and may amplify its healing processes.
- Once all preparatory steps are complete, check into the hospital promptly to ensure doctors have enough time to complete their pre-surgical procedures.
- The Procedure: Meniscus tear surgery is typically performed using minimally invasive tools such as an arthroscope. The procedure may take a couple of hours, after which doctors monitor the patient’s vital signs to ensure the body has responded well to it.
- Patients are typically placed under anesthetic before surgery, causing the patient to become medically unconscious.
- Doctors will begin the surgery with small incisions in the knee, followed by the insertion of a tiny device known as an arthroscope. The arthroscope creates a small tunnel that burrows through the knee, pushing away surrounding tissues.
- The doctors can place several small tools within the arthroscope to directly see what they’re working on and operate on the tissues.
- Depending on the condition of the meniscus, the doctor may remove small portions or the entire thing if the condition is unacceptable.
- Once the surgery is finished, doctors will remove the arthroscope and close the incisions.
- First Few Hours After Surgery: Anesthetic will be applied routinely throughout the first few hours after the surgery. Doctors will monitor vital signs to ensure the surgery is successful. Typically, meniscal surgery is very low-risk and has rare complications.
- 1-2 Days After Surgery: Hospitalization for meniscus surgery is typically short. While regular functionality isn’t immediate, patients will be asked to move the knee within 1-2 days after surgery.
- You will be assigned a physical therapist and begin a routine of light exercises to help stabilize the knee.
- Assisted standing and walking may be asked of you during the sessions immediately following surgery.
- Sometimes, patients may be asked to perform these light tasks on the same day of their surgery.
- One Week Post Operation: Patient activity levels will gradually be increased.
- Once the patient is home, they will be asked to follow the routines their physical therapist taught them and apply any medication the doctors have prescribed.
- Creams, ointments, and medication should be taken as routinely as the doctors have prescribed, and activity levels should be moderate.
- Simple physical therapy such as massage and hot/cold treatments can be applied if medication and rest do not help alleviate post-surgical pain. Consult a doctor if the pain becomes excruciating or if you suffer a knee injury immediately following surgery.
- One Month Post Operation: Light activities can resume, and physical therapy may intensify.
- At this point, the surgical wounds should be healed, and normal activity levels should resume with minimal pain and discomfort.
- Extended use may cause flare-ups of pain, but these bouts of pain should wane over time as the wounds fully recover.
- One Year Post Operation: By this time, the surgical pains should be gone, and normal activity levels should return. While pain and discomfort may still be present, they should be minimal and not prevent functionality.
Regenerative Therapy and Meniscus Tear Surgery Recovery
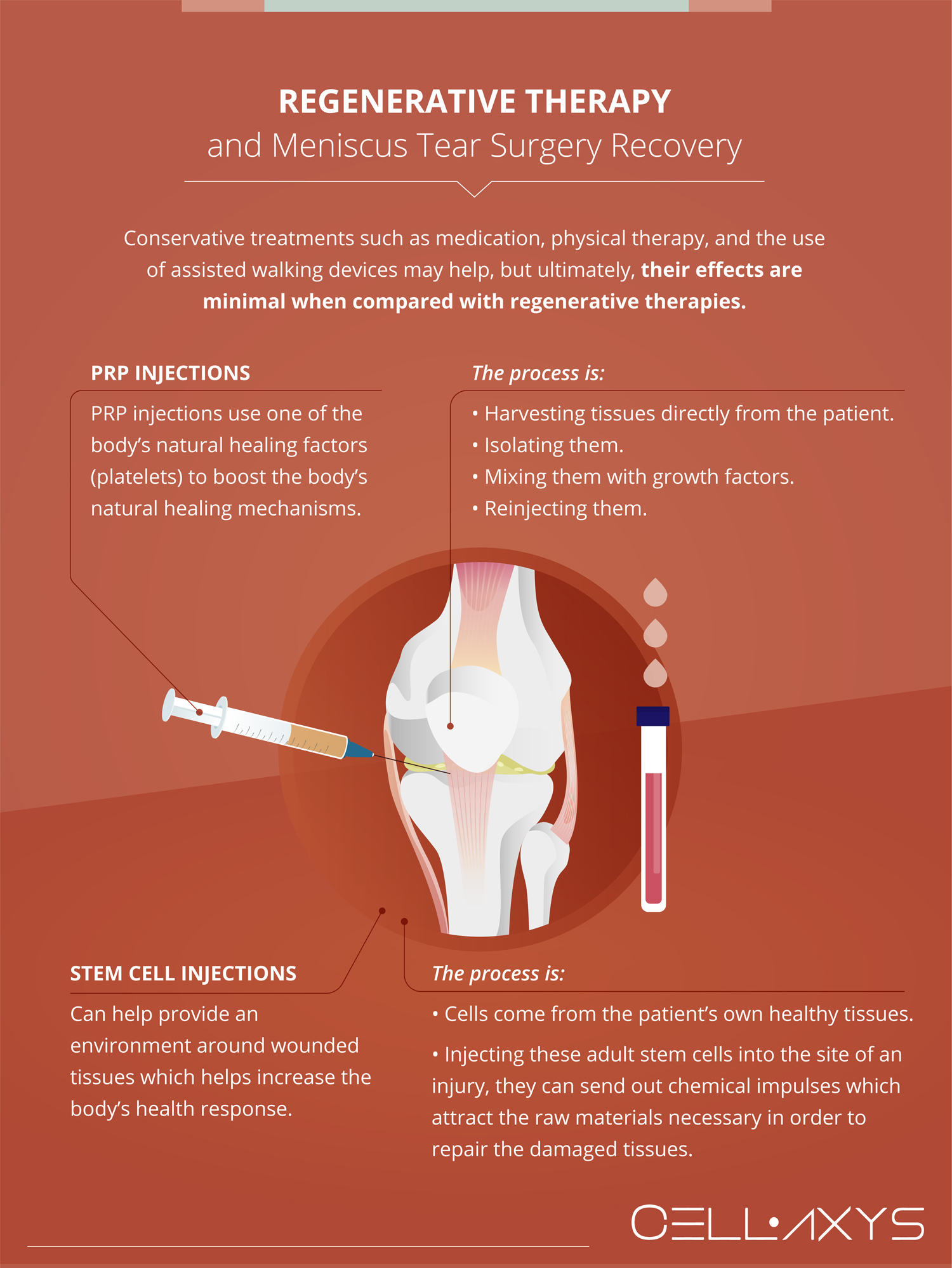
The recovery period for meniscus tear surgery is six weeks to three months, and patient discomfort may last upwards of six months as they acclimate to their new condition. Conservative treatments such as medication, physical therapy, and assisted walking devices such as braces or canes may help. Still, ultimately, their effects are minimal when compared with regenerative therapies.
Applying regenerative therapies, such as platelet-rich plasma (PRP) or autologous stem cell injections, after meniscal tear surgery may reduce recovery times. These treatments can relieve symptoms and amplify the body’s natural healing responses.
PRP injections use one of the body’s natural healing factors (platelets) to boost the body’s natural healing mechanisms. Harvesting and concentrating the platelets can deliver ten growth factors that aid in post-operative healing.
Additionally, autologous stem cell injections can help provide an environment around damaged tissues, which helps increase the body’s recovery/healing response. The source material for these injections is taken directly from the patient’s healthy tissues. Fat and bone marrow can be processed with new methods developed into concentrated, stem cell-rich tissue within the last decade.
By injecting these adult stem cells into the site of an injury, the cells can aid in the repair and recovery of the damaged tissues. Combining both therapies relieves symptoms, boosts healing, and decreases overall recovery time.
Signs You’re Ready to Return to Work
Before you return to work, you must be sure your joint is completely healed. Some signs indicate you are good to go up and running.
- Subsequently, the pain and swelling will diminish so you can walk, sit, and stand without discomfort.
- Your knee will feel stronger, and you can get up and work without pain.
- You can also move, lift, and bend without pain or straining the joint.
- Follow your doctor’s recommendation and make sure to get medical clearance before you head to work.
- Claim your medical clearance before resuming work. Your surgeon will assess your healing progress, strength, and mobility before giving you the green light.
- Don’t return to work before your body is ready. Doing so can lead to many complications, including reinjury, tissue tearing, and long-term joint issues.
Sources
Footnotes
- Nakayama H, Kanto R, Kambara S, Kurosaka K, Onishi S, Yoshiya S, Yamaguchi M. Clinical outcome of meniscus repair for isolated meniscus tear in athletes. Asia-Pacific journal of sports medicine, arthroscopy, rehabilitation and technology. 2017;10:4-7.
- Brindle T, Nyland J, Johnson DL. The meniscus: review of basic principles with application to surgery and rehabilitation. Journal of athletic training. 2001;36(2):160.
- Harput G, Guney-Deniz H, Nyland J, Kocabey Y. Postoperative rehabilitation and outcomes following arthroscopic isolated meniscus repairs: a systematic review. Physical Therapy in Sport. 2020;45:76-85.
- Willinger L, Herbst E, Diermeier T, Forkel P, Woertler K, Imhoff AB, Achtnich A. High short-term return to sports rate despite an ongoing healing process after acute meniscus repair in young athletes. Knee Surgery, Sports Traumatology, Arthroscopy. 2019;27:215-22.
- Stärke C, Kopf S, Petersen W, Becker R. Meniscal repair. Arthroscopy: the journal of arthroscopic & related surgery. 2009;25(9):1033-44.
- Fried JW, Manjunath AK, Hurley ET, Jazrawi LM, Strauss EJ, Campbell KA. Return-to-play and rehabilitation protocols following isolated meniscal repair—a systematic review. Arthroscopy, Sports Medicine, and Rehabilitation. 2021;3(1):e241-7.
- Spang III RC, Nasr MC, Mohamadi A, DeAngelis JP, Nazarian A, Ramappa AJ. Rehabilitation following meniscal repair: a systematic review. BMJ open sport & exercise medicine. 2018;4(1):e000212.
References
- Meniscus Tears. OrthoInfo. Accessed 2/23/2024.
- Meniscus Surgery. Cleveland Clinic. Accessed 2/23/2024.
- What is the Recovery Time for Meniscus Tear Surgery? SportsMD.com. Accessed 2/23/2024.
CELLAXYS does not offer Stem Cell Therapy as a cure for any medical condition. No statements or treatments presented by Cellaxys have been evaluated or approved by the Food and Drug Administration (FDA). This site contains no medical advice. All statements and opinions are provided for educational and informational purposes only.
Dr Pejman Bady
Author
Dr. Pejman Bady began his career over 20 years ago in Family/Emergency Medicine, working in fast-paced emergency departments in Nevada and Kansas. He has served the people of Las Vegas as a physician for over two decades. Throughout this time, he has been met with much acclaim and is now the head of Emergency Medical Services in Nye County, Nevada. More about the doctor on this page.
Dr Pouya Mohajer
Contributor
Pouya Mohajer, M.D. is the Director of Spine and Interventional Medicine for CELLAXYS: Age, Regenerative, and Interventional Medicine Centers. He has over 20 years of experience in pain management, perioperative medicine, and anesthesiology. Dr. Mohajer founded and is the Medical Director of Southern Nevada Pain Specialists and PRIMMED Clinics. He has dedicated his career to surgical innovation and scientific advancement. More about the doctor on this page.