Published on: March 6, 2020 | Updated on: November 3, 2024
Deciding to undergo surgery can be difficult, as there is a lot you need to consider. From aftereffects and risks to the efficacy and costs, it’s natural to be worried before going under the knife.
Fortunately, there are many effective alternatives to meniscus or knee surgeries, which eliminate the need for all the hassle. However, these methods sometimes don’t give the desired results, making surgery your last resort.
One of the main questions many patients ask their doctors during the consultation is, “How to treat knee pain that persists one year after meniscus surgery?” Well, the answer varies, depending on various factors.
Do you have Knee Pain?
Fill out the form below to schedule your FREE virtual consultation
What is the Meniscus?
The knee is the largest joint in the body, making it most susceptible to injury. Since it carries most of the body’s weight, injury and pain can occur due to disruptions of the intricate structures that keep the joint together.
To know how the meniscus works, we must first understand the structure of the joint. The knee is one of the body’s most complex joints. It is a joint that connects the thigh bone (femur) to the shin bone (tibia). The other bones that make up the knee joint are the fibula (the smaller bone that runs beside the tibia) and the patella (kneecap).
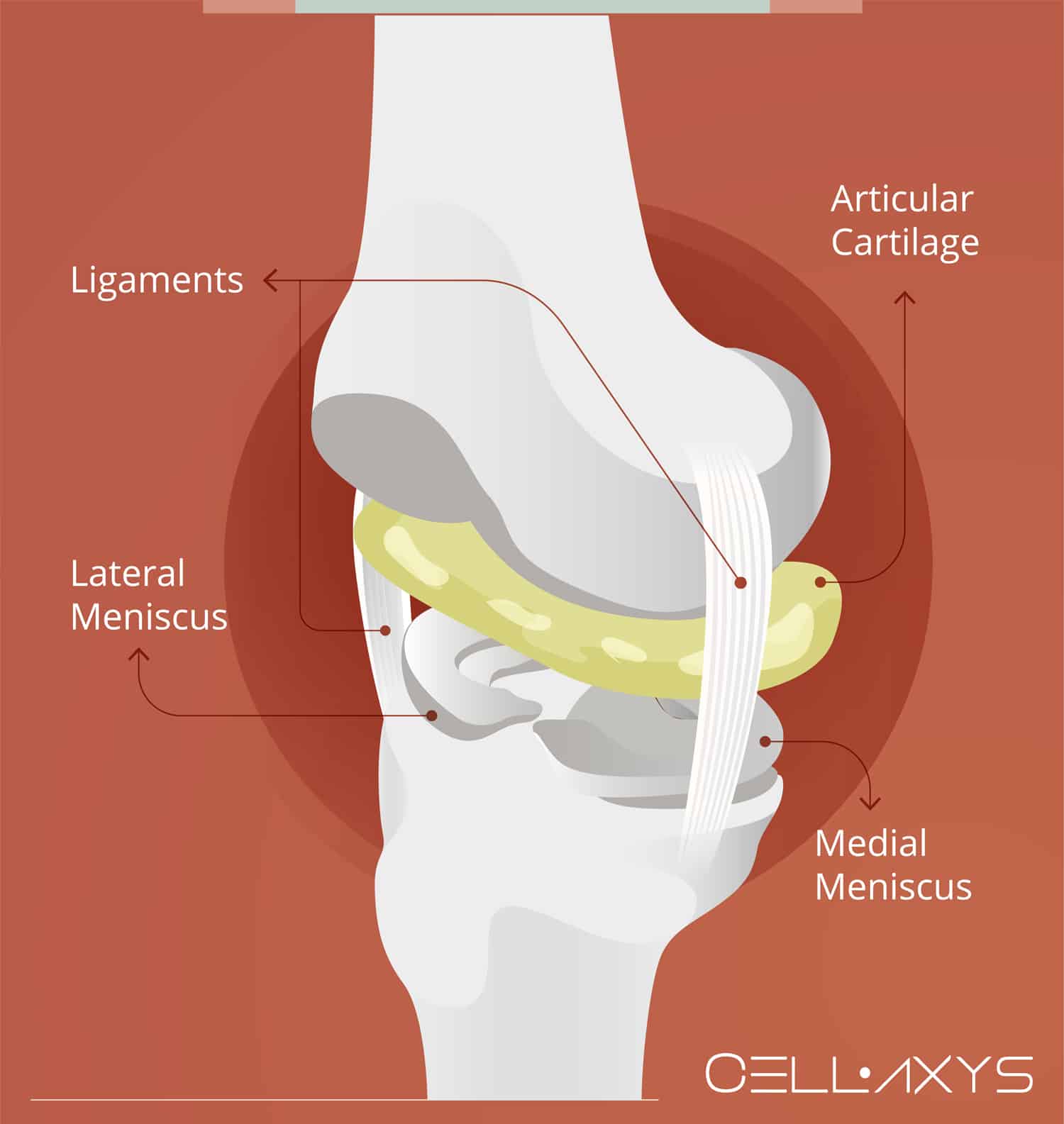
Soft tissues surrounding the joint include ligaments, muscles, and tendons. Each structure provides a service—ligaments connect the thigh bone to the shin bone and provide stability. Muscles help with the motion of the joint while supporting it as well. Tendons form connections like ligaments, but they also connect muscles to bones.
Cartilage is between the knee bones, which protects from the bones – without cartilage, bones can rub against one another, causing pain and damage to the surrounding area. There are two significant types of cartilage in the knee joint, each with a particular function:
- Articular Cartilage: Located at the ends of the bone, articular cartilage acts as a barrier between bones. This prevents the discomfort that comes with bones rubbing against each other. Articular cartilage can become damaged from long-term use or sudden injury.
- Meniscus: Located between the thigh and shin bones, the meniscus absorbs shock in the joint. There are two types of the meniscus: medial and lateral. The medial meniscus is larger and more prone to injury. The lateral meniscus is smaller and less prone to injury, though it is not immune. The meniscus also provides stability to the joint and helps with weight distribution.
Cartilage injuries can occur during sports, a car accident, or a fall, among many other incidents. Meniscus tears occur most commonly in athletes who participate in high-impact sports that involve twisting the knee. There is also a risk of cartilage deteriorating over time naturally or from repetitive motion. Symptoms may vary, but there are some prominent ones to look out for:
- Popping noises
- Pain
- Difficulty with balance
- Less range of motion
Depending on the cause, symptoms may become manageable and worsen over time or occur suddenly. Pain could be short, sharp, or more of a dull ache—or anywhere between. Some minor injuries can heal independently, but how to treat knee pain that persists one year after meniscus surgery?
This signifies that it is time to consult a doctor, especially when the pain begins to impede daily activities.
How a Meniscus Injury is Treated?
The first step to treating knee pain is finding the cause. Injury to the meniscus can often be spotted when a doctor performs a small series of tests to diagnose it. This may include watching the patient walk, bending the knee, and finding where the pain is located.
Doctors may order an MRI or other imaging techniques such as X-rays or CT Scans. The images can give doctors a clear idea of what is causing knee pain and from where. An MRI is a standard technology used to diagnose a meniscus injury because it takes an image of the soft tissue, which includes cartilage.
Once the diagnosis is particular, doctors can devise a treatment plan specific to the patient’s needs. A meniscus injury can vary in severity. Some tears are minor and cause very few symptoms, while others can be more severe and may require surgery.
Treating a meniscus injury generally includes a few important steps before surgery is considered:
- Pain Management: Many patients take over-the-counter drugs to relieve pain, such as Ibuprofen or Naproxen. Relieving pain can make it easier to perform daily activities that would otherwise be too difficult.
- RICE: Rest, Ice, Compression, and Elevation can help reduce swelling while providing comfort.
- Corrective Gear: Knee braces can help keep the joint stable while it heals. Assistive devices such as crutches or a cane may be used to put less weight on the joint.
- Physical Therapy: Certain exercises can help restrengthen the joint after an injury, significantly if some muscles have atrophied during the healing process. Some of the goals of physical therapy are to restore range of motion, build strength, and reduce pain during certain activities.
Patients who go through these treatments may have some success, as the body is capable of healing itself. Some injuries are beyond natural repair, however, and require surgical intervention.
What Happens During Meniscus Surgery?
Surgery is often considered a “last resort” for patients with knee pain. Though many patients begin to recover after only six weeks, it can be a complex process. Every surgery has risks that should be discussed thoroughly with doctors and surgeons before the operation begins. Some common concerns involve receiving anesthesia and the risks of infection or blood clots.
The most common form of meniscus surgery is done arthroscopically. This means that the surgery begins with a small incision, into which surgeons insert a tiny camera and tools. The tools are then used to repair the damage, which may involve shaving away damaged tissue or repairing a tear.
As arthroscopy is a minimally invasive surgery, the recovery time is much shorter than that of a total knee replacement or other, more involved procedures. Many patients choose to try this form of surgery so that damage can begin to heal again. As with any treatment, however, there is a risk that symptoms do not go away, even after surgical intervention.
How Can Knee Pain Persist After Surgery?
There are several reasons why knee pain may continue after meniscus surgery. These reasons may vary depending on what was accomplished during the surgery. These are the most common reasons why pain persists:
Delayed Healing
Despite undergoing surgery, people still stay in pain due to incomplete or delayed healing of the tissues around the knee.
This may be due to poor blood supply to the knee, making it take longer to heal. At times, the meniscus may not have fully repaired, leaving damaged tissue that causes discomfort. Scar tissue may also develop, causing further pain and stiffness.
Osteoarthritis or Cartilage Damage
Osteoarthritic patients suffer from severe symptoms after the surgery. Since the meniscus is partly removed and repaired during the surgery, it can accelerate arthritis or wear out of the knee joint, leading to pain.
Some cartilage may also be left exposed after the surgery, which can cause clicking or grinding and pain in the knee while standing or when exerting weight on it.
Nerve or Soft Tissue Damage
During surgery, the tissues around the joint get damaged. This can cause the nerves around the knee to get irritated, leading to sharp, shooting pains and tingling in the area, which can last longer even after the surgery.
Bursitis is another condition that occurs after surgery and causes pain and discomfort.
Reinjury
After the surgery, the knee becomes weaker and more vulnerable to reinjuries. Activities that require twisting or heavy lifting can also tear the meniscus.
The tear strains the ligaments and causes further pain. At times, the pain is worsened by high-impact sports exercises and injuries like cartilage breakdown, tendonitis, and stress, which can lead to additional pain.
Poor Rehabilitation
Patients must follow the instructions of doctors and physical therapists closely after an operation. This is a vulnerable time for the knee, and exercising in specific ways or developing a limp could cause more damage to the joint. This can be prevented by listening closely, practicing, and sticking to the regimen, even when it’s complicated.
Developing Arthritis
Arthritis occurs when the cartilage lining the joint bones begins to deteriorate. Meniscus surgery does not address the loss of articular cartilage. Specific damage to the cartilage that occurs due to arthritis can be difficult and even impossible to repair using arthroscopic surgery.
Damage may occur after surgery, in which case patients face the option of a total knee replacement surgery.
The vast majority of patients with continued knee pain after meniscus surgery have pain associated with the loss of articular cartilage. In these cases, autologous stem cell-rich bone marrow or adipose (fat) tissue is an excellent option.
Damaged Meniscus
Many surgeries performed to repair the meniscus involve simply removing damaged tissue. When this occurs, the meniscus becomes smaller but must absorb the same amount of shock. This can lead to retreading of the meniscus, as well as increased pain and discomfort.
Though these are some common reasons why pain persists, several others, such as swelling and infection, should also be considered. Doctors will order new tests to determine the cause of persistent pain, which may include blood and image tests.
Some medical professionals are skeptical of the efficacy of meniscus surgery, with some studies implying that it is ineffective and unnecessary. Luckily, there are alternative treatments for meniscus injury that offer promising results for short- and long-term treatment.
Other Complications
Other complications include infection after meniscus surgery, which can cause persistent pain, swelling, and further complications. The materials used during surgery, like the switchers and implants, can also cause this comfort and inflammation.
Yet another condition is Deep Vein Thrombosis, which can cause blood clots in the leg, causing pain and swelling.
Alternative Treatments for Knee Pain
Regenerative medicine is an emerging field of medical science that offers long-term and effective treatment for meniscus tears and many other conditions. These treatments work well on soft tissue, making them a good option for repairing damage to many types of cartilage.
These treatments use a patient’s cells to enhance natural healing processes in the body. When damage occurs anywhere, the body sends specific cells to the area to begin making repairs. These treatments have found a way to inject a more densely packed version of some of these cells into the area where injury exists.
Two of the most promising treatments offered at CELLAXYS are platelet-rich plasma (PRP) therapy and autologous stem cell therapy, specifically using your fat or “adipose tissue.” The process for both is similar, beginning with a sample from the patient, which most often comes as a blood draw. The samples are then processed to concentrate the healing properties and transplanted into the area where healing is most necessary.
Doctors use imaging technology such as ultrasound or fluoroscopy to guide the needle to the location where its effects will be strongest. Both outpatient procedures can most often be performed in about two hours.
Though PRP and stem cell therapies can ease pain and discomfort in patients after surgery, they may also be a good option for someone who is considering surgery. Some patients can surpass the need for meniscus surgery, eliminating the need to cut and remove tissue that could otherwise be used to support the knee and absorb shock.
Preventive Measures
You can help prevent long-term pain by taking specific preventive steps like:
- Indulge in low-impact sports like cycling, swimming, and walking. But do not strain the knee.
- Work on exercises that build strength in the leg muscles. Strong muscles will support the knee joint and reduce pressure on the meniscus.
- Minimize strenuous exercises like jumping, running, and twisting that could strain the knee and cause reinjuries.
- Maintain a healthy body weight to reduce knee pain and damage.
- Consume healthy foods such as leafy greens and fish for healthy bones and to minimize inflammation.
- Wear knee braces and compression sleeves for support.
- Take time out for stretching exercises to keep the muscles and body flexible around the knee.
Sources
Footnotes
- Stärke C, Kopf S, Petersen W, Becker R. Meniscal repair. Arthroscopy: the journal of arthroscopic & related surgery. 2009;25(9):1033-44.
- Tayfur B, Charuphongsa C, Morrissey D, Miller SC. Neuromuscular function of the knee joint following knee injuries: does it ever get back to normal? A systematic review with meta-analyses. Sports medicine. 2021;51:321-38.
- MacFarlane LA, Yang H, Collins JE, Guermazi A, Jones MH, Teeple E, Xu L, Losina E, Katz JN. Associations among meniscal damage, meniscal symptoms and knee pain severity. Osteoarthritis and cartilage. 2017;25(6):850-7.
- Vaquero J, Forriol F. Meniscus tear surgery and meniscus replacement. Muscles, ligaments and tendons journal. 2016;6(1):71.
- Post WR. Anterior knee pain: diagnosis and treatment. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2005;13(8):534-43.
References
- Causes and treatment for knee pain 1 year after meniscus surgery. Medical News Today. Accessed 9/4/2023.
- 5 Long-Term Problems After Meniscus Surgery. Verywell Health. Accessed 9/4/2023.
- What Is the Recovery Time for a Meniscus Tear Without Surgery?. Healthline. Accessed 9/4/2023.
CELLAXYS does not offer Stem Cell Therapy as a cure for any medical condition. No statements or treatments presented by Cellaxys have been evaluated or approved by the Food and Drug Administration (FDA). This site contains no medical advice. All statements and opinions are provided for educational and informational purposes only.
Dr Pouya Mohajer
Author
Pouya Mohajer, M.D. is the Director of Spine and Interventional Medicine for CELLAXYS: Age, Regenerative, and Interventional Medicine Centers. He has over 20 years of experience in pain management, perioperative medicine, and anesthesiology. Dr. Mohajer founded and is the Medical Director of Southern Nevada Pain Specialists and PRIMMED Clinics. He has dedicated his career to surgical innovation and scientific advancement. More about the doctor on this page.
Dr Pejman Bady
Contributor
Dr. Pejman Bady began his career over 20 years ago in Family/Emergency Medicine, working in fast-paced emergency departments in Nevada and Kansas. He has served the people of Las Vegas as a physician for over two decades. Throughout this time, he has been met with much acclaim and is now the head of Emergency Medical Services in Nye County, Nevada. More about the doctor on this page.