Published on: December 11, 2019 | Updated on: February 3, 2025
The spine provides the structural support and balance needed to maintain our upright posture. This places incredible pressure on the bones (vertebrae) within the spine, especially during bouts of extreme physical exertion.
Fortunately, each vertebrae in the spine is cushioned by special, pillow-like discs that help absorb the shocks of daily movements.
What is a Herniated Disc?
A herniated disc, more commonly called a slipped or ruptured disc, occurs when the soft or gel-like center of the spinal disc pushes through a crack or tear in the outer layer.
This causes a change in the surrounding nerves, which either get irritated or compressed, causing general discomfort and pain.
When the inner material escapes its protective casing, it pressurizes the surrounding nerves. A fall, car accident, or other traumas can lead to its escape and damage the disc.
Another common reason is aging. Our discs lose their water content and elasticity as we age, making them prone to tears and disc degeneration.
Other likely causes include:
- Putting repetitive strain on the spine by lifting, bending, and twisting.
- Some individuals may have a genetic disposition or weaker disc and spine structures.
- Poor lifestyle choices or habits like obesity, sedentary habits, or smoking as well could lead to disc degeneration.
These discs comprise two layers: an inner, softer layer that provides most of the shock-absorbing cushion and a more rigid outer layer that acts as a gasket to protect the inner layer and absorb the heaviest wear on the spine.
Herniated discs occur when a portion of the inner layer of the disc is pushed out through a tear or rupture in the tough outer layer. As the outer layer degrades, more inner tissue is expelled, and the displaced tissue creates uncomfortable pressure points throughout the spine.
These pressure points upset the spine’s nerves, leading to bouts of pain, which increase in severity as more tissue escapes the disc.
People with herniated discs can experience relief through physical therapy or medication, but over time, surgical intervention, such as a discectomy, will be necessary to provide long-lasting relief. Additionally, stem cells for herniated discs are a popular way to decrease recovery times from discectomies and increase the surgery’s positive effects.
Anatomy of the Spinal Discs
In clinical terminology, the spine is divided into three major sections: the cervical (upper), thoracic (middle), and lumbar (lower) spine. Each section is made up of several interlocking bones called vertebrae, and between each vertebrae lies a fibrous disc that helps cushion the pressures of our everyday movements within the spine.
The discs have two parts. The tough outer layer, the annulus fibrosus, provides a gasket to keep the soft, gel-like center tissue (nucleus pulposus) from spilling. In addition to detaining the nucleus, the annulus helps attach the vertebrae above and below the disc with tiny endplates of tough, cartilaginous fibers.
Together, these discs help support our everyday movements and act as the body’s major carrier of axial load.
As we age and the outer layer degrades, the inner nucleus begins to spill out through ruptures in the annulus. When the outer discs rupture and the inner disc spills out, this can lead to bouts of pain, swelling, and reduced flexibility and range of motion.
Once a disc is ruptured, it will never fully heal. Medication and physical therapy can be used to help treat and manage the symptoms of a herniated disc, but they will never truly restore its health.
Typically, surgical intervention through a discectomy (removing the disc from the spine) is the only way to get long-lasting relief after a disc has become herniated. If this is the case, recovery can be long, and if the proper care is not taken to ensure the surgery is as successful as possible, recovery times can be even longer.
As with all health problems, diagnosis is the first step in successfully treating a herniated disc.
Symptoms of Herniated Disc
The symptoms of a Herniated disc vary per person and location. But some common signs to watch out for include:
- A localized pain in the back, lower back, or neck
- Pain down the arms or legs
- Numbness or tingling sensation in the arms, legs, or other parts of the body
- General weakness in the body caused by compressed nerve
- Difficulty in holding objects and walking
- Loss of bladder or bowel control
- Increase in severity or duration of bouts of pain
- Mobility issues in the back
- Back pain or sensitivity due to changes in the environment – rain, higher elevations, colder climate
- Back pain which interferes with sleep cycles
- Previous injury to the back, which did not heal properly
- Tingling, aching, redness, or burning in the affected area
If these symptoms persist and affect your everyday functionality, a discectomy may seem a viable option to return to normal activity levels.
Stages of Diagnosis for Herniated Discs
Many factors determine the complexity of surgery for herniated discs, and each of these factors ultimately determines how long recovery will take.
Discectomies may be minimally invasive, requiring only a short hospital stay and applying medication and physical therapy routines, or they may be more involved and require more advanced post-surgical intervention.
However, diagnosis is critical before any surgery. A routine examination allows doctors to assess the tissues in the spine and determine whether more conservative approaches can alleviate pain and enable patients to reach their functional goals.
The health care providers usually conduct a series of tests based on the patient’s history. Then, they may order an imaging test for the herniated disc.
The first steps in diagnosis are a complete evaluation of the patient’s medical history and a routine physical examination. These exams will give the healthcare provider an idea of possible causes of the patient’s pain and help them determine whether a herniated disc is likely.
Physical Examination
The first part of the testing is the physical examination. The doctors check for muscle strength, body sensory response, and reflexes.
They check specific movements or positions to see how badly the nerve is affected.
Imaging Tests
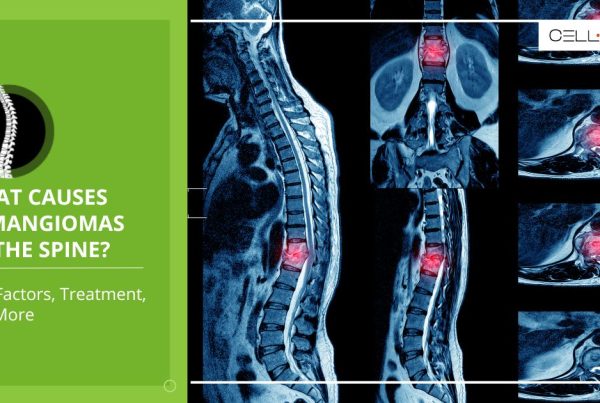
Next, the doctors order an MRI, the most effective way to check soft tissues like nerves and discs.
Then, a CT scan may also be done. This can provide detailed spine images and is mainly ordered if the MRI is unavailable.
Further, the doctors may order X-rays to rule out conditions like fractures or spinal misalignment.
- X-Ray: Small amounts of radiation produce images of the bones within the body. X-rays are typically preliminary tests to rule out other causes of back pain besides herniated discs.
- MRI or CT Scan: These tests are especially important for herniated disc diagnosis as they can show whether the spinal canal has narrowed – a key symptom of herniation.
- Myelogram: During a myelogram, doctors inject a special dye into the spinal canal that shows up on a CT scan. The dye spreads through the spine and helps doctors pinpoint the size and location of a herniation.
Other Tests
Electromyography, or EMG, is also conducted to check the extent of damage in the nerves and muscles.
An electromyogram (EMG) helps doctors assess the damage around the herniation to understand how involved the discectomy will be. By placing small needles into various muscles throughout the spine and measuring electrical activity, doctors can evaluate the condition of the nerves within the muscle.
If several nerves are affected, the discectomy may be a vastly more complex surgery than if not.
Making the Decision
While your discectomy may not be highly invasive, it still requires a thorough examination of all possible consequences. While doctors may recommend a particular treatment, the decision to pursue it is always left to the patient.
Financial status, age, relative success rates, and familial considerations all play critical roles in determining whether or not the patient should have surgery. If a lengthy recovery period is suspected, this may also play a major role in deciding the surgery.
If surgical intervention is chosen, the patient should take special care in the days and weeks before the surgery to ensure all matters are in order. It is best to talk to the doctor to uncover all the steps and research online to discover what the doctor may have missed.
Age and Health
An important consideration here is that young individuals and those in good physical health usually recover quicker due to better tissue regeneration and muscle strength.
Similarly, older adults or individuals suffering from chronic conditions like diabetes or osteoporosis may have slower healing and prolonged recovery.
Factors Influencing Recovery Time from a Herniated Disc
Now, one of the most commonly asked questions by those suffering from herniated discs is how long it will take to recover from it.
The truth is that recovery depends on several factors. Every individual and patient is different, so recovery is unique to them and depends on the severity of the condition and its location. The type of treatment plan being followed.
Moreover, personal health and lifestyle choices also play a significant role.
As a rule, here’s a general timeline for the recovery period:
Severity of the Condition
Small tears or minor herniation usually take around 4 to 6 weeks following conservative treatment like physical therapy, rest, and anti-inflammatory medicines. The pain is mild in these conditions and, hence, can be controlled with conservative treatment therapy.
Severe herniation that causes nerve compression and spinal eligibility can take months to heal at times; it will require surgery.
Location of the Herniation
The herniation may be located on the cervical spine, which can cause arm pain, weakness, or numbness. The recovery time may also be short due to less body pressure on the area.
- Mid Back or Thoracic Spine: Herniation can have long recovery times due to limited mobility in the area.
Lumbar Spine: The lumbar spine is the most common location for herniation. Recovery takes much longer because this area bears much of the body’s weight and may be subject to mechanical stress.
Herniated Disc Surgery: A Timeline
The trajectory for a specific discectomy varies from patient to patient, but there are critical points every discectomy will have. The following is an outline of these points, and though they may not reflect your exact procedure, they should give you a good idea of what you can expect.
This guideline is intended to help patients in their decision-making process and allow them to understand what they can expect while going through the surgical process. Take these guidelines with caution and be sure to reach out to your doctor with any questions you may have.
Preparing for Herniated Disc Surgery
Any successful surgery begins with an adequate amount of preparation. These preliminary steps help promote the well being a patient before and after surgery and may boost its success rate.
- Schedule bloodwork: though your health care team will do everything in their power to identify any risk factors before surgery, performing a blood analysis is by far the most important pre-surgery step. Analyzing a patient’s blood will help doctors determine if any outside risk factors might hinder their ability to perform the surgery well.
- Preliminary “travel” processes: Arrange for rides to and from the hospital, update your emergency contact information, request the necessary time off work, and prepare luggage (toiletries and clothes) to last through the days after surgery.
- Doctor’s notes: stop or start taking any medications your doctor recommends. Do not eat in the hours leading up to the surgery. Refrain from alcohol or drug use. Maintain an adequate sleep schedule.
- Research your medications: Inquire which type of anesthetic will be used and see how it will affect you. Ask about which medications your doctor will be prescribing for post-surgical recovery and learn about their side effects.
- Donate blood: in some cases, the surgical process may cause excessive blood loss. While doctors should have stores of donated blood at your disposal, it may be a cheaper, more effective option to donate your own in the weeks leading up to your surgery. Consult your doctor to see if this may be an option.
- Check-in: with all preparatory steps complete, check into the hospital on time to ensure there is adequate time for all pre-surgical procedures and any final checkups the doctors must do.
The Procedure
Discectomies may last several hours depending on the location of the herniated disc and the health of the surrounding tissues. Surgery may take longer if the patient is older or if they are in poor health.
- First, an incision is made somewhere along the spine. Discectomies can be performed anywhere from the neck (cervical) to the low back (lumbar).
- In an open discectomy, the muscles are retracted and held in place.
- The spinal nerve is then retracted to one side and held in place. This is an especially important step as the spinal nerve is responsible for motor, sensory, and autonomic signals between the spinal cord and the body.
- In a minimally invasive procedure, a small incision is made and doctors use special tools to bore through the muscles and create a tunnel to access the damaged disc. Special tools are used to remove the disc and the tools used to tunnel through the muscles are removed.
- In some cases, a spinal fusion may be performed in unison with the discectomy to help stabilize the spine. While spinal fusion may increase the overall time of the procedure, it may decrease recovery periods. During this process, the doctor uses special equipment to fuse two vertebrae into a single bone. Fusion is rarely needed in cases of herniated discs, but you may want to talk to your doctor to see if it will be right for you.
- Finally, the surgeon will remove the affected disc(s), replace the retracted nerve, muscles, and bone, and sew the incision closed.
The first few hours after surgery
Anesthetic will be applied routinely throughout the first few hours after the surgery. Doctors will monitor vital signs to ensure the surgery was successful.
- 1-2 days after surgery: Recovery for herniated disc surgery is typically short. While regular functionality isn’t immediate, patients will be asked to move within 1-2 days after surgery.
- A physical therapist will be assigned to you and begin a routine of light exercises to ensure that post-surgical trauma is minimal.
- Assisted stretching and light periods of standing and walking may be asked of you during the sessions immediately following surgery.
- In some cases, patients may be asked to perform these light tasks involving the back on the same day of their surgery.
- 1 week after surgery: Patient activity levels will gradually be increased and the patient will be released upon approval by the physical therapist.
- Once the patient is home, they will be asked to follow the routines their physical therapist taught them as well as apply any medication the doctors have prescribed.
- Creams, ointments, and medication should be taken as routinely as the doctors have prescribed and activity levels should be moderate.
- Simple physical therapy such as massage and hot/cold treatments can be applied if medication and rest do not help alleviate post-surgical pain. Consult a doctor if the pain becomes excruciating or if you suffer back injury immediately following surgery.
- 1 month after surgery: Light activities can resume and physical therapy may intensify.
- At this point, the surgical wounds have still not fully healed, but normal activity levels should resume, albeit with minimal pain and discomfort.
- Extended use may cause flare-ups of pain, but these bouts of pain should wane over time until the wounds fully recover.
- 1 year after surgery: By this time the surgical pains should be gone, and normal activity levels should return. While pain and discomfort may be inevitable, these pains should not be so excruciating that they prevent functionality. Monitor any back injuries thoroughly and report them to doctors immediately following signs of excess damage or decreased functionality.
Treatments
The treatment plan for herniated discs can go anywhere from conservative regenerative, and surgical.
Physical Therapy
In physical therapy, targeted exercises and stretches help improve the body’s mobility and strength. They also speed up recovery and are successful for mild to moderate cases.
Medicines
Non-steroidal anti-inflammatory drugs, NSAIDs, and muscle relaxants can help manage pain and inflammation.
Surgery
Different surgical plans are recommended depending on the severity of the patient’s underlying conditions and other aspects.
Microdiscectomy is a minimally invasive surgical procedure where part of the herniated disc is removed. This type of recovery lasts 6 to 8 weeks, and many patients feel immediate relief after the surgery.
Laminectomy is a sort of more invasive procedure where part of the vertebra is removed to relieve pressure on the spine.
Recovery takes 3 to 6 months, by which patients regain complete functionality.
Tips for Faster Recovery from a Herniated Disc
Recovering from herniated discs requires a shift in lifestyle. Patients must make healthier life choices to speed up recovery and prevent complications.
- Stick to the treatment plan, which includes physical therapy and prescribed exercises.
- As your physical therapist recommends, focus on low-impact exercises and activities like walking, swimming, or stretching.
- Follow up with your healthcare provider routinely to ensure you recover well and adjust your treatment plan as needed.
- Use ergonomic furniture and ensure your workplace and seating supports the spinal alignment.
- Refrain from bending, twisting, and heavy weightlifting that can worsen the injury.
- Follow a balanced and healthy diet plan incorporating leafy greens, berries, fish, and nuts
- Drink lots of water to stay hydrated
Herniated Disc Surgery and Regenerative Medicine
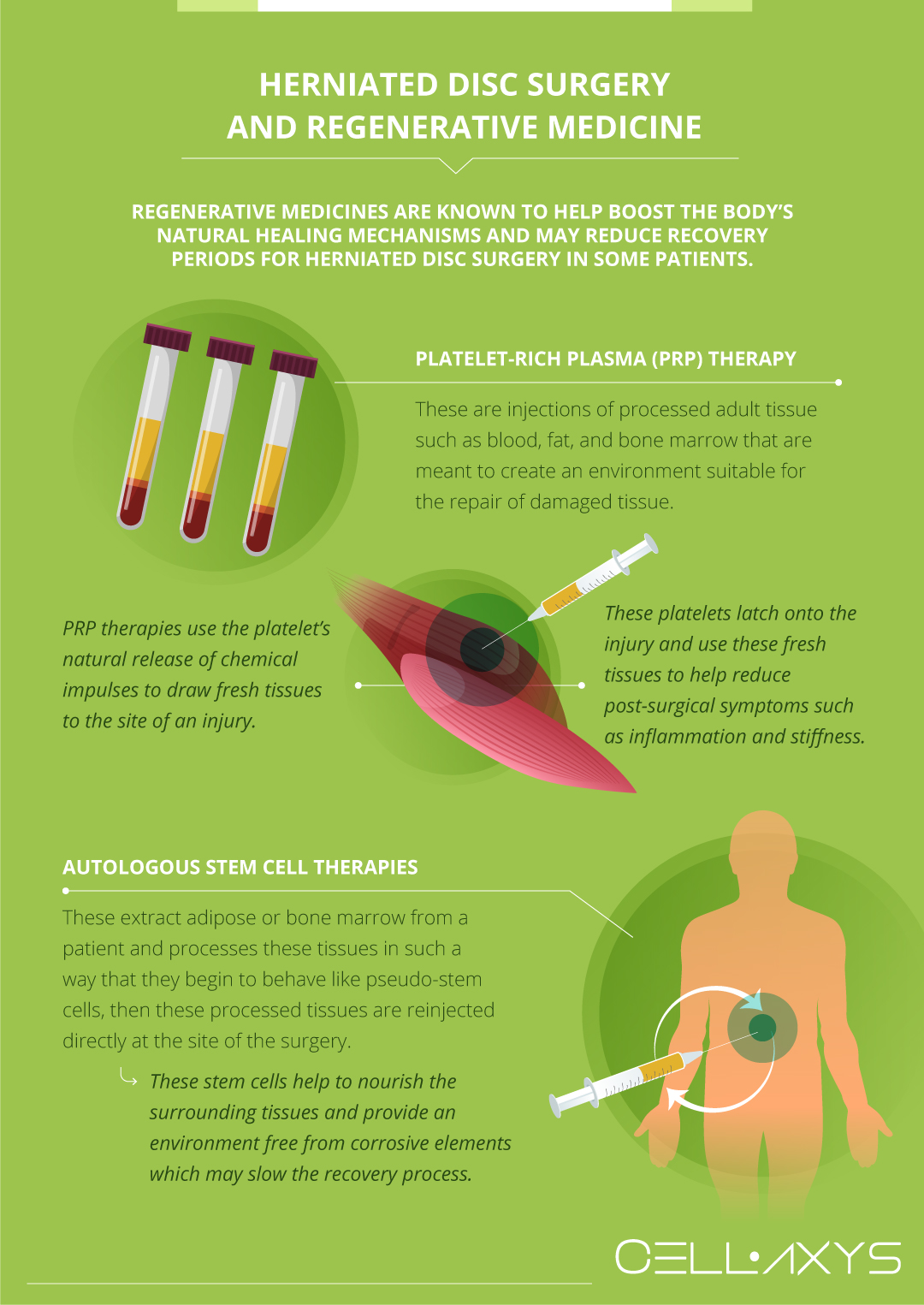
It is necessary to rest and monitor your post-surgical symptoms to prevent further damage to the spine’s discs. Regenerative medicines help boost the body’s natural healing mechanisms and may reduce recovery periods for herniated disc surgery in some patients.
Regenerative therapies, such as cell-based and platelet-rich plasma (PRP) therapy, involve injecting processed adult tissue, such as blood, fat, and bone marrow, to create an environment suitable for repairing damaged tissue.
At CELLAXYS, we perform both types of regenerative therapies.
PRP Therapy
This treatment isolates the platelets from the patient’s blood plasma. These platelets are then processed in a centrifuge and reinjected into the patient’s injury site.
Platelets are the healing components in our body that act as the first line of defense against injuries. They contain 10 Growth Factors, release chemical signals, and produce a sticky web called fibrin to support the development of new tissues in the injury site.
A high number of platelets in the injury site means speedy recovery.
Cell-Based Therapies
These treatments extract healthy cells from the patient’s adipose (fat) tissue or bone marrow, process them, and then reinject them directly at the surgery site to help boost the patient’s healing responses.
The procedure is called a Minimally Manipulated Adipose Tissue (MMAT) transplant, and the cells are harvested from the adipose tissue. If they are taken from the bone marrow, the process is called bone marrow concentrate (BMAC).
PRP therapy is performed within 45 minutes, while cell-based therapies take about 1.5 to 2 hours to complete. Both are outpatient procedures, meaning you can go home after the process. The doctors use live X-rays and ultrasounds to detect the exact transplant location.
By using these therapies in unison, many patients have found relief from post-surgical symptoms and a shorter recovery. To learn more about how regenerative therapies can help you recover from herniated disc surgery more quickly, contact the CELLAXYS offices today to schedule a consultation.
Sources
Footnotes
- Jordon J, Konstantinou K, O’Dowd J. Herniated lumbar disc. BMJ clinical evidence. 2009;2009.
- Dedering Å, Gnospelius Å, Elfving B. Reliability of measurements of endurance time, electromyographic fatigue and recovery, and associations to activity limitations, in patients with lumbar disc herniation. Physiotherapy Research International. 2010;15(4):189-98.
- Otani K, Arai I, Mao GP, Konno S, Olmarker K, Kikuchi S. Experimental disc herniation: evaluation of the natural course. Spine. 1997;22(24):2894-9.
- Altun I, Yüksel KZ. Lumbar herniated disc: spontaneous regression. The Korean Journal of Pain. 2017;30(1):44-50.
- Kasnakova P, Mihaylova A, Petleshkova P. Comprehensive rehabilitation of herniated disc in the lumbar section of the spine. Biomedical Research. 2018;29(14):3002-5.
- Jacobs WC, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, Ostelo R, Verhagen A, Koes B, Peul WC. Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. European Spine Journal. 2011;20:513-22.
References
- Will my herniated disc heal on its own? Harvard Health Publishing. Accessed 2/23/2024.
- Signs Your Herniated Disc Is Healing. HealthCentral. Accessed 2/23/2024.
- Back Pain: Everything You Need to Know. HealthCentral. Accessed 2/23/2024.
CELLAXYS does not offer Stem Cell Therapy as a cure for any medical condition. No statements or treatments presented by Cellaxys have been evaluated or approved by the Food and Drug Administration (FDA). This site contains no medical advice. All statements and opinions are provided for educational and informational purposes only.
Dr Pouya Mohajer
Author
Pouya Mohajer, M.D. is the Director of Spine and Interventional Medicine for CELLAXYS: Age, Regenerative, and Interventional Medicine Centers. He has over 20 years of experience in pain management, perioperative medicine, and anesthesiology. Dr. Mohajer founded and is the Medical Director of Southern Nevada Pain Specialists and PRIMMED Clinics. He has dedicated his career to surgical innovation and scientific advancement. More about the doctor on this page.
Dr Pejman Bady
Contributor
Dr. Pejman Bady began his career over 20 years ago in Family/Emergency Medicine, working in fast-paced emergency departments in Nevada and Kansas. He has served the people of Las Vegas as a physician for over two decades. Throughout this time, he has been met with much acclaim and is now the head of Emergency Medical Services in Nye County, Nevada. More about the doctor on this page.