Published on: July 22, 2019 | Updated on: February 3, 2025
Spinal fusion is a surgical procedure that is used to treat abnormalities within the spine. The little bones that make up your spinal column are called vertebrae. The procedure is aimed to permanently fuse two or more vertebrae in your spine, preventing them from moving.
Intervertebral disks divide these vertebrae, which stack on top of each other. These bones guard your spinal cord, which transmits and receives data from your brain to the rest of your body.
Your vertebrae may slide against each other more than they should due to a variety of medical issues. This can cause discomfort by stretching your surrounding nerves, ligaments, and muscles. If you have arthritis in your spine, for example, moving your vertebrae against each other may cause pain. By immobilizing one or more of your vertebrae, spinal fusion may be able to relieve your discomfort.
How Spinal Fusion Works
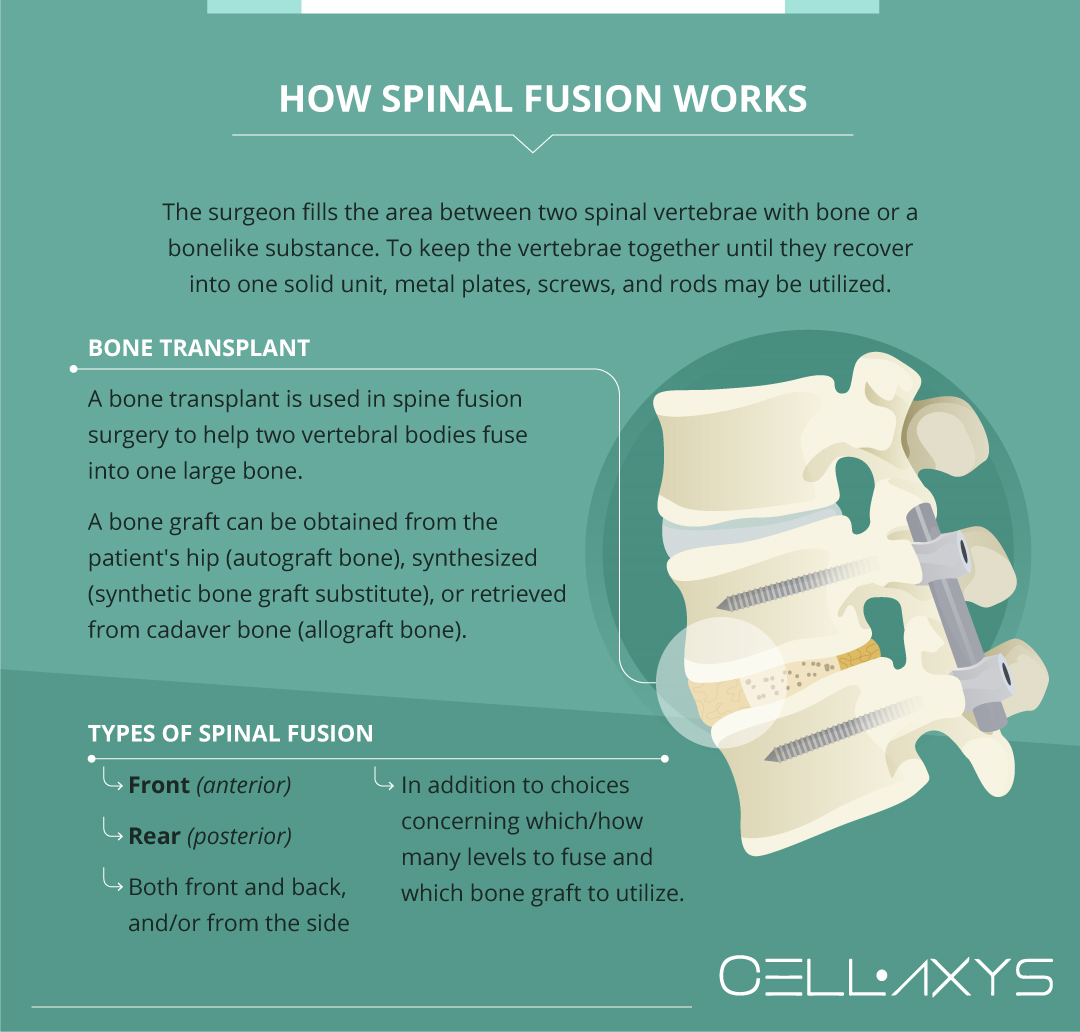
Techniques for spinal fusion are aimed to mirror the natural healing process of damaged bones. During spinal fusion, your surgeon fills the area between two spinal vertebrae with bone or a bonelike substance. To keep the vertebrae together until they recover into one solid unit, metal plates, screws, and rods may be utilized.
There is a disk gap in the front and paired facet joints in the rear at each level of the spine. These structures allow for various degrees of motion when they work together. An L4-L5 (lumbar segment 4 and lumbar segment 5) spinal fusion is a one-level spinal fusion since two vertebral segments must be fused to halt mobility at one segment. A 2-level fusion is an L4-L5, L5-S1 fusion.
A bone transplant is used in spine fusion surgery to help two vertebral bodies fuse into one large bone. During spinal fusion surgery, a bone graft can be obtained from the patient’s hip (autograft bone), synthesized (synthetic bone graft substitute), or retrieved from cadaver bone (allograft bone).
There are various types of spinal fusions, including fusions using surgical approaches from the front (anterior), rear (posterior), both front and back, and/or from the side, in addition to choices concerning which/how many levels to fuse and which bone graft to utilize.
Why Get Spinal Fusion Surgery?
The movement of vertebrae is a symptom of several illnesses that cause back and/or neck discomfort. The following are some of the difficulties that may be alleviated by spinal fusion:
- Degenerative disk disease
- Herniated disk
- Spondylolisthesis
- Scoliosis
- Spinal stenosis
- Tumor
- Vertebrae fracture
- Infection
It might take a long time to get from basic back issues to spinal fusion surgery. Surgery is normally not recommended until other less intrusive therapies have failed, except for a shattered spine.
The first-line therapies for back pain include medication and physical therapy. The choice to have spinal surgery is based on the patient’s medical history, as well as testing such as an X-ray, MRI, and a physical exam.
How to Prepare for Spinal Fusion Surgery
Preparing for spinal fusion surgery involves a few important steps to set you up for a smoother recovery.
Here’s a detailed guide to help you get ready.
Comprehensive Medical Checkup
A healthcare team assesses your overall health with certain medical and lab tests. Generally, they check for underlying issues like high blood pressure, clotting problems, or kidney function irregularities – things you might not even be aware of – to make sure your body is ready for surgery.
Review Medications and Supplements
Be open about everything you take, from medications to supplements. That’s because certain drugs, like blood thinners, may need to be paused to prevent complications.
Anesthesia and Blood Planning
Although most spinal fusion surgeries don’t require a blood transfusion, your doctor may still discuss options like donating your own blood beforehand, just in case.
This is a precautionary step for your peace of mind. Besides, this is also the right time to share any past experiences with anesthesia. For instance, if you’ve encountered certain allergies or nausea during anesthesia, make sure you’re transparent about it.
Nicotine and Lifestyle Adjustments
Nicotine, in any form, can sabotage your recovery. It disrupts blood flow and impairs healing. What’s even worse is that it weakens your ability to regenerate bone tissue (something critical for the success of spinal fusion).
Therefore, if you smoke or vape, your doctor will likely insist on quitting weeks before surgery. For those who need a helping hand, know that numerous doctors offer resources to make this step achievable.
Pre-Surgery Cleansing and Fasting
Your doctor will give you a specific cleaning routine for the day before the surgery. They might, for instance, ask you to use a special antibacterial soap to minimize infection risk.
Additionally, fasting for a specific number of hours (usually overnight) keeps your stomach empty for anesthesia, which eventually reduces potential complications.
Support Planning at Home
It goes without saying that you won’t be able to do everything independently right after surgery.
Even simple tasks like lifting or driving may be off-limits for a while. Therefore, make sure you have someone – a friend, a family member or a caregiver – to help with household chores.
What to Expect on the Day of Your Spinal Fusion Recovery
The day of your spinal fusion is carefully structured to prioritize your peace of mind. From the moment you step into the hospital to the moment you’re wheeled into the operating room, a highly trained team will take every precaution to prepare you and keep you at ease. Here’s a detailed look at what happens.
In the Preparation Area
- Final health and history review. A nurse will go through your medical history one last time. They’ll confirm emergency contact details and double-check that no critical information is overlooked.
- Meeting your anesthesia team. You’ll have a detailed conversation with the anesthesia team. They’ll explain the type of anesthesia being used and give you an opportunity to ask questions. If you’re feeling nervous, this is the team that will reassure you; they’re experts at keeping you comfortable.
- Signing consent and marking the surgery site. Your surgeon, or a member of their team, will confirm that you’ve signed the consent form. Then, they’ll carefully mark the surgical site. This might feel like a small step, but it’s part of a larger system designed to avoid errors.
- Placing the IV line. A healthcare provider will insert an intravenous (IV) line into a vein, typically in your arm or hand. This will be used to deliver fluids and antibiotics during surgery.
In the Operating Room
- Vital monitoring for your safety. Once you’re in the operating room, the surgical team will attach monitors to track your heart rate, blood pressure, oxygen levels, and more. These tools allow them to monitor your condition in real-time.
- Meeting the full surgical team. Alongside your surgeon, you’ll meet an anesthesiologist, surgical assistants, scrub nurses, and circulator nurses. It might surprise you to see how many professionals are involved but everyone is plays a role to keep you safe during the procedure.
- Pre-surgery safety checklist. Before any incision is made, the team conducts a detailed safety check. This includes verifying your identity and the procedure plan to confirm everything is correct before proceeding.
Anesthesia administration. Once all the safety checks are completed, you’ll receive anesthesia through your IV. It works quickly and gently, easing you into a deep sleep.
What to Expect During Spinal Fusion Surgery
Surgeons execute spinal fusions while you’re under anesthesia, so you’re completely unaware of what’s going on. Various procedures for doing spinal fusion surgery have been devised by surgeons. The procedure employed by the surgeon is determined by the position of the fused vertebrae, the cause for the fusion, and, in certain cases, your overall health and body form.
The surgery involves:
- Incision: The surgeon makes an incision in one of three places to obtain access to the vertebrae being fused: in your back over your spine, in your neck, on either side of your spine, or in your throat or abdomen to reach the spine from the front.
- Preparing the bone graft: Bone grafts that connect two vertebrae might come from a bone bank or your own body, most typically your pelvis. The surgeon will make an incision above your pelvic bone, take a little portion, and then seal the wound.
- Fusion: Between the vertebrae, the surgeon inserts bone graft material to permanently fuse them. While the bone graft cures, metal plates, rods, or screws, can keep the vertebrae together.
Some surgeons employ synthetic material instead of bone transplants in certain circumstances. These synthetic chemicals aid to increase bone development and accelerating vertebral fusion.
How Long Does the Surgical Procedure Take?
While the surgery itself usually takes between one to five hours, the total time in the operating room can be longer.
Generally, the variability depends on the complexity of your case. For example, a straightforward fusion involving one level of the spine might be on the shorter end, while addressing multiple levels or more complex conditions could extend the duration.
Your surgeon will walk you through the specifics based on your unique situation.
It’s also important to note that preparation and safety checks (think anesthesia administration and positioning) add to the overall time. While waiting can feel daunting, know that every moment is focused on getting it right for you.
Complications
As with any surgery, there are risks associated with spinal fusion. Your doctor will discuss each of the risks with you before your procedure and will take specific measures to help avoid potential complications. Potential risks and complications of spinal fusion include:
- Infection: To reduce the risk of infection, antibiotics are given to the patient before, during, and often after the operation.
- Bleeding: A small amount of bleeding is to be expected, although it is rarely severe. Before a spinal fusion, it is typically not essential to donate blood.
- Pain at graft site: A small minority of patients will have ongoing discomfort at the location of the bone transplant.
- Recurring symptoms: Some people may have a repeat of their initial symptoms. There are several reasons for this. If your initial symptoms return, tell your doctor so they can figure out what’s causing them.
- Pseudarthrosis: This is a situation in which the bone development is insufficient to make a firm fusion. Pseudarthrosis is more prone to occur in smokers. Diabetes and advanced age are two further factors. Pseudarthrosis can also be caused by moving too soon before the bone has had time to fuse. A second operation may be required if this occurs.
- Nerve damage: It’s conceivable that nerves or blood vessels will be damaged as a result of this procedure. These consequences are extremely uncommon.
- Blood clots: The production of blood clots in the legs is another unusual consequence. If they break off and migrate to the lungs, they represent a serious threat.
Recovery
Recovery after spinal fusion surgery may be difficult and painful, and the time it takes to feel like yourself again is dependent on several factors, including your health, age, and the breadth of the treatment.
- The first 2-4 days after spinal fusion: The recovery process following spinal fusion surgery begins with a stay in the hospital for the first 2-4 days. During this period, medical staff and surgeons closely monitor patients to manage any pain or discomfort and ensure that the procedure has not resulted in any problems. Physical therapists will work closely with patients to educate them on how to securely get in and out of bed, dress, stand, sit, and walk so that they do not twist or bend, which can cause back pain and delay the healing process.
- 1-4 weeks after spinal fusion: The major objective at this period is to strike a balance between resting and keeping a safe level of exercise. This aids in the healing and fusing of the vertebrae, as well as the strengthening of the back muscles. Patients must follow numerous critical activity limits during this stage of rehabilitation, including no twisting or bending of the back and no lifting anything weighing more than 10 pounds. This is the beginning of outpatient physical treatment and a gradual return to normal activities of daily living, such as driving and working.
- 1-3 months after spinal fusion: At this moment, the fused parts of the spine begin to grow together. Though physicians typically advise patients to start slowly, it’s critical to maintain a high level of exercise throughout this time. Still, some actions should be avoided, such as bending, carrying significant weight, or doing anything that causes a twisting motion. A physical therapist could suggest that you do some new activities. The patient should be able to resume normal activities such as driving, light housework, and even working (as long as no strenuous exercise is involved).
- 3-6 months after spinal fusion: Exercise must take the lead in the recovery process after 3 months of healing and a gradual increase in physical activity. Twisting, bending, and heavy lifting should be avoided, but stretching, aerobics, and other exercises should be increased. Many patients are apprehensive that the fusion may be harmed. However, at this stage, movement is beneficial for promoting healing and strengthening the fusing bones.
- 6 months to one year: The outcome of the spinal fusion treatment and whether the vertebrae fused as anticipated will be determined by an orthopedic expert. The patients are now able to resume their daily routine. This includes tasks that require bending, twisting, and lifting, and patients may usually resume practically all of their previous activities – with a few acceptable limits. High-impact activities, such as extreme sports, full-contact sports, and others, are generally discouraged by doctors, at least in the near term.
In most cases, the vertebrae will fully heal and fuse after a total of 12-18 months. Furthermore, if there was any nerve injury, the nerve tissue may take as many as two years to repair and return to normal.
Alternative Treatments: Regenerative Medicine
A lengthy recovery time combined with potential complications makes spinal fusion surgery a tough decision. Many patients may seek to find a less invasive treatment for spinal issues and regenerative medicine can provide just that.
Regenerative medicine and orthobiologic therapies are quickly gaining traction in the medical field because of the high success rate. CELLAXYS offers two of these types of treatment:
- Cell-based therapies. These treatments start with harvesting healthy cells or “autologous” tissues from the patient’s own body. These cells are processed to become more concentrated and are reinjected into the patient’s injury site. Depending on your condition, the doctor will go for Minimally Manipulated Adipose Tissue (MMAT) transplant, which extracts healthy cells from your adipose (fat) tissue, or Bone Marrow Concentrate (BMAC), which harvests highly concentrated cells from your bone marrow. These methods are performed within 1.5 to 2 hours. The doctor will put you under anesthesia and use a live X-ray or ultrasound to locate the injury site.
- Platelet-rich plasma (PRP) therapy. This treatment starts by drawing blood from the patient and isolating platelets from the plasma. These platelets are injected into the patient’s injury site to promote healing. Platelets release 10 Growth Factors to stimulate the development of healthy tissues. They also send chemical signals to attract growth cells from the blood and produces a sticky web-like structure called fibrin. Fibrin supports the growth of new, healthy tissues in the body. PRP therapy is a popular treatment for several spine, orthopedic, and sports injuries. The procedure completes within 45 minutes.
Both of these therapies are outpatient procedures with minimal recovery periods and side effects. Patients typically experience swelling and soreness after injection, though this goes away within a week.
In the case of a damaged disk, the stem cells would signal the body to help rebuild the cartilage around it. This procedure only involves injection, making it much less invasive than spinal fusion surgery. Furthermore, it is typically less expensive.
Sources
Footnotes
- Tarpada SP, Morris MT, Burton DA. Spinal fusion surgery: a historical perspective. Journal of orthopaedics. 2017;14(1):134-6.
- Lipson SJ. Spinal-fusion surgery—advances and concerns. New England Journal of Medicine. 2004;350(7):643-4.
- Raizman NM, O’Brien JR, Poehling-Monaghan KL, Warren DY. Pseudarthrosis of the spine. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2009;17(8):494-503.
- Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA. Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine. 2007;32(3):382-7.
- Bohl DD, Webb ML, Lukasiewicz AM, Samuel AM, Basques BA, Ahn J, Singh K, Vaccaro AR, Grauer JN. Timing of complications after spinal fusion surgery. Spine. 2015;40(19):1527-35.
References
- Spinal fusion. Mayo Clinic. Accessed 2/25/2024.
- Spinal Fusion. OrthoInfo. Accessed 2/25/2024.
- All About the L4-L5 Spinal Segment. SPINE-Health. Accessed 2/25/2024.
- Anesthesia. MedlinePlus. Accessed 2/25/2024.
CELLAXYS does not offer Stem Cell Therapy as a cure for any medical condition. No statements or treatments presented by Cellaxys have been evaluated or approved by the Food and Drug Administration (FDA). This site contains no medical advice. All statements and opinions are provided for educational and informational purposes only.
Dr Pouya Mohajer
Author
Pouya Mohajer, M.D. is the Director of Spine and Interventional Medicine for CELLAXYS: Age, Regenerative, and Interventional Medicine Centers. He has over 20 years of experience in pain management, perioperative medicine, and anesthesiology. Dr. Mohajer founded and is the Medical Director of Southern Nevada Pain Specialists and PRIMMED Clinics. He has dedicated his career to surgical innovation and scientific advancement. More about the doctor on this page.
Dr Pejman Bady
Contributor
Dr. Pejman Bady began his career over 20 years ago in Family/Emergency Medicine, working in fast-paced emergency departments in Nevada and Kansas. He has served the people of Las Vegas as a physician for over two decades. Throughout this time, he has been met with much acclaim and is now the head of Emergency Medical Services in Nye County, Nevada. More about the doctor on this page.









